Antihistamine Eye Drops Comparison Tool
Your Needs
Results
Select your needs above to see your recommendation.
Antihistamine eye drops are ophthalmic medicines designed to block histamine receptors on the surface of the eye, giving fast relief from itching, redness and watery discharge caused by allergic conjunctivitis. Unlike oral antihistamines that affect the whole body, these drops stay where they’re needed, so systemic side effects such as drowsiness are rare. If you’ve ever scratched your eyes during pollen season, you know how frustrating the symptoms can be - luckily a few drops can calm the reaction in minutes.
How topical antihistamines work
When an allergen lands on the eye, mast cells release histamine, which binds to H1 receptors on nerve endings and triggers the classic itching sensation. A topical antihistamine competes for those H1 receptors, preventing histamine from attaching and stopping the itch signal. Many modern drops, such as olopatadine, also act as mast‑cell stabilizers, reducing the amount of histamine released in the first place.
Common formulations and what sets them apart
Three agents dominate the market today:
- Ketotifen - first approved in 1993, available as a 0.025% solution (OTC brands Zaditor, Alaway). It works within 5‑15 minutes and needs twice‑daily dosing for most users.
- Olopatadine - launched in 1996, comes in 0.1%, 0.2% and 0.7% concentrations. The 0.7% version (Pataday) offers once‑daily 24‑hour relief and combines antihistamine with mast‑cell stabilization.
- Azelastine - a 0.05% solution (Optivar) that acts within 3 minutes but usually requires twice‑daily use.
All three contain the preservative benzalkonium chloride (≈0.01%) unless you choose a preservative‑free single‑use vial, which is a good option for people who notice stinging after a few weeks.
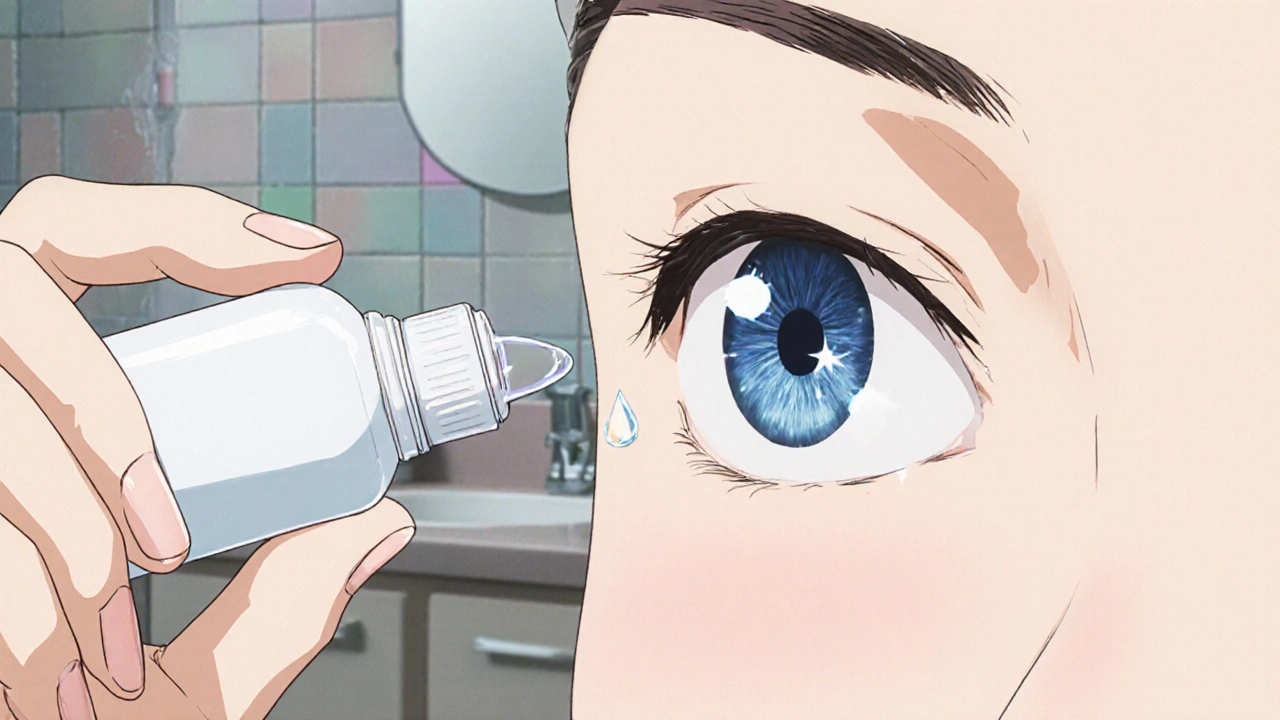
Proper technique - get the most out of each drop
- Wash your hands thoroughly with soap and water.
- Shake the bottle if the label says to do so (most ketotifen and azelastine bottles require a gentle shake).
- Tilt your head back slightly, pull down the lower eyelid to create a small pocket.
- Hold the bottle close to the eye (about 1‑2 cm) without touching the tip to any surface.
- Squeeze one drop into the pocket, then close your eye gently for about 30 seconds. Press the inner corner of the eye (punctal occlusion) to reduce systemic absorption.
- If you wear contact lenses, wait 10‑15 minutes before reinserting them.
- Store the bottle at room temperature (15‑30 °C) and replace it according to the expiration date - most multi‑dose bottles are good for 30 days after opening.
Refrigerating the drops for a few minutes can cut down the initial sting that 40% of new users report.
Side effects you should monitor
Most people experience only mild, temporary sensations, but be alert for:
- Burning or stinging - usually fades within a minute; more common with azelastine and preservative‑containing bottles.
- Redness persisting beyond 72 hours - a sign that the problem might not be allergic and needs a professional eye exam.
- Increased intra‑ocular pressure (IOP) - rare, but can happen after 12‑16 weeks of uninterrupted use, especially in glaucoma‑prone patients.
- Allergic reaction to the preservative - swelling, itching or watery discharge that worsens after a week of daily use.
If any of these symptoms sustain, stop the drops and book an appointment with an ophthalmologist.
OTC vs. prescription - what’s the real difference?
OTC drops (ketotifen 0.025%) are affordable ($15‑25 per 2.5 mL bottle) and available without a doctor’s note, making them perfect for occasional flare‑ups. Prescription strengths (olopatadine 0.7%, azelastine 0.05%) cost more ($85‑120) but offer longer wear time and often contain fewer preservatives.
Choosing wisely depends on three factors:
- Frequency of symptoms - daily sufferers benefit from once‑daily olopatadine.
- Tolerance to preservatives - preservative‑free single‑use vials cost about $4‑5 each but eliminate irritation.
- Underlying eye conditions - anyone with a history of glaucoma, cataract surgery or chronic dry eye should discuss options with a specialist before using any antihistamine drop.
Special situations
Allergic conjunctivitis is the most common indication, but antihistamine drops won’t cure bacterial or viral infections. If redness is accompanied by thick discharge, fever or vision changes, seek medical care immediately.
For contact‑lens wearers, the timing rule (wait 10‑15 minutes) is crucial. A 2023 survey of 200 ophthalmologists found that 12% of lens‑related complications were linked to re‑inserting lenses too soon after drop administration.
Children as young as six can use OTC ketotifen, but dosage‑frequency instructions should be followed exactly. Some pediatric formulations (Children’s Alaway) come in smaller 1 mL bottles to help parents control usage.
Pregnant or breastfeeding patients should talk to their doctor; while systemic absorption is minimal, safety data are limited.
Comparison of the three most popular drops
| Attribute | Ketotifen (0.025%) | Olopatadine (0.7%) | Azelastine (0.05%) |
|---|---|---|---|
| OTC status | Yes (Zaditor, Alaway) | No (prescription only) | No (prescription only) |
| Onset of relief | 5‑15 min | 3‑5 min | 3 min |
| Duration of action | 8‑12 h | 16‑24 h | 8‑10 h |
| Dosing frequency | Twice daily | Once daily | Twice daily |
| Typical price (US) | $15‑25 | $85‑120 | $70‑100 |
| Preservative | Benzalkonium chloride 0.01% | Often preservative‑free (single‑use) or BAK 0.01% | Benzalkonium chloride 0.01% |
Practical tips to avoid common pitfalls
- Never share your bottle - contamination rates climb to 24% after one week of multi‑use.
- Keep the dropper tip clean; wipe it with a tissue if it contacts your eye or skin.
- Stop using the drops if redness persists beyond three days; a different diagnosis may be needed.
- Schedule an eye exam after 12 weeks of continuous use, especially if you have risk factors for glaucoma.
- For severe seasonal peaks, combine a topical antihistamine with a cold compress for extra comfort.
Future outlook
The market for ocular allergy relief is growing fast, projected to hit $2.14 billion globally in 2022 and keep expanding as pollen seasons lengthen. New nano‑emulsion forms of olopatadine promise 16‑hour relief with less stinging, while research into ketotifen‑dexamethasone combos may open doors for treating severe keratoconjunctivitis.
Regardless of the brand you pick, the core rule stays the same: use the drops correctly, watch for warning signs, and involve an eye‑care professional when symptoms linger.
How quickly do antihistamine eye drops start working?
Most drops begin to reduce itching within 3‑5 minutes; ketotifen may take up to 15 minutes, while olopatadine and azelastine often feel relief in under 5 minutes.
Can I use antihistamine drops if I wear contact lenses?
Yes, but wait 10‑15 minutes after applying the drop before putting lenses back in. This prevents the medication from being wiped away and reduces the risk of irritation.
Are there any risks for people with glaucoma?
Long‑term, unchecked use can raise intra‑ocular pressure in a small percentage (3‑5%) of glaucoma‑susceptible patients. Schedule an eye exam after 12 weeks of continuous use.
Should I choose preservative‑free drops?
If you notice burning after a few days or have a history of eye‑surface sensitivity, preservative‑free single‑use vials are worth the extra cost. They eliminate benzalkonium chloride irritation.
When should I stop using OTC drops and see a doctor?
If redness or itching lasts more than 72 hours, if you develop a thick yellow discharge, or if vision becomes blurry, stop the drops and get an eye‑care evaluation right away.


I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.