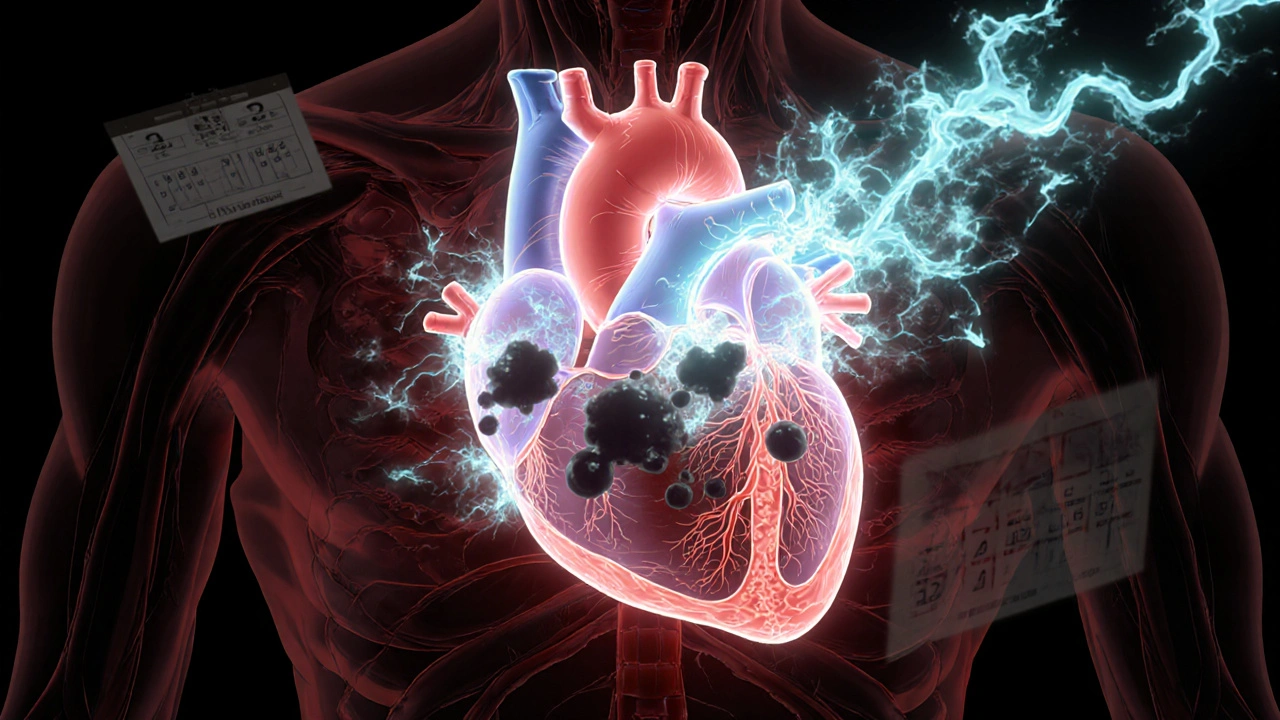
Every year, over 900,000 people in the U.S. have a stroke caused by a blood clot. For many, that clot forms because of atrial fibrillation - a chaotic heartbeat that lets blood pool and thicken in the heart. Left untreated, this condition can turn deadly. But here’s the good news: taking the right blood thinner can cut your stroke risk by two-thirds. The question isn’t whether you need one - it’s which one works best for you.
What Are Blood Thinners Really Doing?
Blood thinners don’t actually thin your blood. They stop clots from forming by blocking key proteins in your clotting system. If you have atrial fibrillation, your heart doesn’t pump smoothly. Blood sits still in the upper chambers - the atria - and starts to clot. Those clots can break loose, travel to your brain, and cause a stroke. That’s where anticoagulants come in.
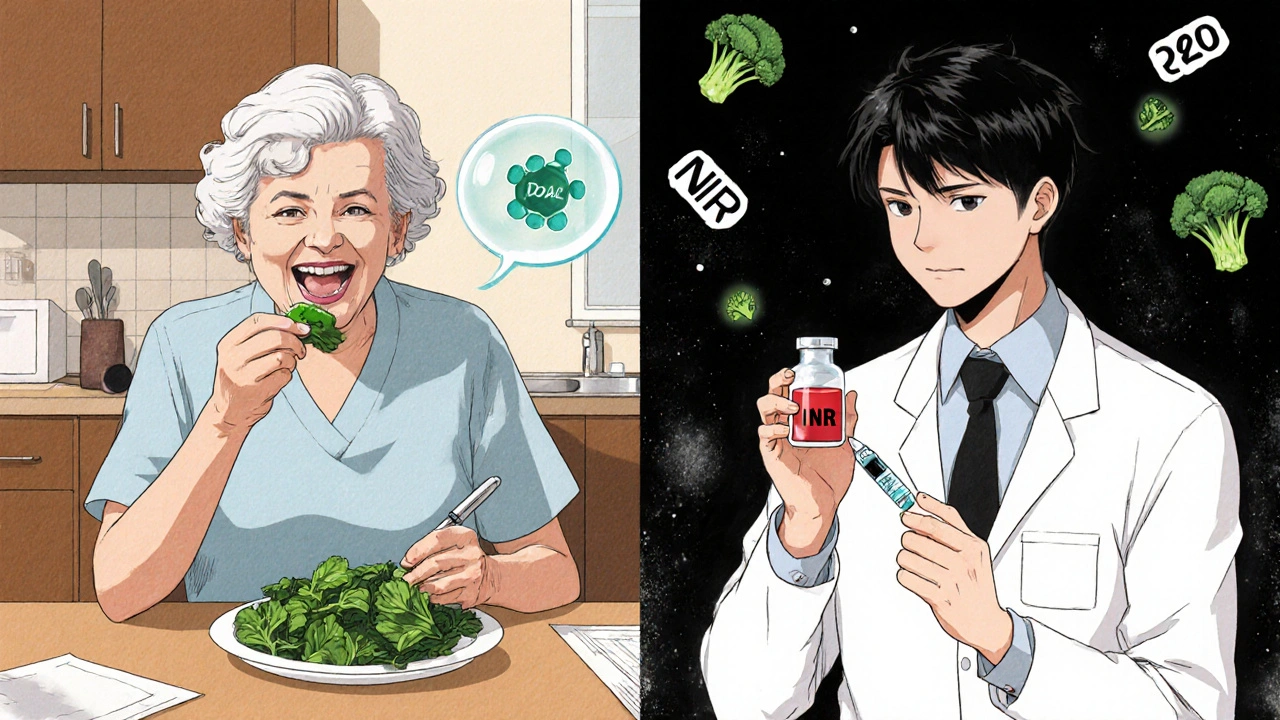
There are two main types: warfarin and the newer DOACs (direct oral anticoagulants). Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting factors. But that also means your diet matters. Eating a big plate of kale or broccoli can make warfarin less effective. That’s why people on warfarin need frequent blood tests - usually every 2 to 4 weeks - to check their INR levels. The goal? Keep it between 2.0 and 3.0. Most people struggle to stay in that range. In real-world settings, only about half maintain it above 65% of the time.
DOACs - like apixaban, rivaroxaban, dabigatran, and edoxaban - work differently. They target specific clotting factors directly. Apixaban and rivaroxaban block factor Xa. Dabigatran blocks thrombin. No vitamin K interference. No dietary restrictions. And no routine blood tests. That’s why, in patient surveys, 78% of DOAC users say they prefer their medication over warfarin.
Which One Is Better? The Evidence
A 2022 analysis of nearly 268,000 patients found apixaban reduced stroke and major bleeding more than warfarin. Specifically, it cut major bleeding by 31%. Another review of over 2.2 million patients showed DOACs lowered stroke risk by 23%, reduced death by 29%, and slashed major bleeding by 32% compared to warfarin.
One of the biggest wins? Intracranial bleeding - bleeding inside the skull. That’s the kind that can kill or leave you disabled. DOACs cut that risk by more than half. Warfarin users have a much higher chance of this happening.
But not all DOACs are the same. Dabigatran has the highest rate of stomach upset - about 32% of users report nausea or bloating. Apixaban has the lowest bleeding risk among DOACs and is often the top pick for older adults or those with kidney issues. Rivaroxaban is taken once a day, which helps with adherence. Edoxaban is the least prescribed, mostly because it’s still brand-name in many places.
Warfarin still has its place. If you have a mechanical heart valve - especially a mitral valve - DOACs are dangerous. The RE-ALIGN trial showed dabigatran increased clots in these patients. Warfarin is also preferred if you have severe kidney failure (CrCl under 15 mL/min), because DOACs build up in your system. And if you’re on multiple medications that interact with DOACs - like certain antifungals or HIV drugs - warfarin might be safer because you can adjust it with blood tests.
Cost and Accessibility
Back in 2020, DOACs cost $600 to $700 a month. That was a barrier for many, especially seniors on fixed incomes. But everything changed in 2023 and 2024. Generic versions of apixaban, rivaroxaban, and dabigatran hit the market. As of early 2024, generic apixaban costs $450-$500. Rivaroxaban is around $580. Dabigatran is $550. Brand-name edoxaban? Still $600.
Warfarin? It’s $650 for the drug - but you have to add in 12 to 16 INR tests a year. Each test is $15 to $25. So total cost? Around $650 to $700. And that doesn’t count missed work, travel to clinics, or the stress of constant monitoring.
In the U.S., 78% of new prescriptions for atrial fibrillation are now DOACs. Apixaban alone makes up 42% of that market. In Europe, it’s even higher - 85%. But in low-income countries, warfarin still dominates because DOACs are too expensive.
Who Should Take What?
Your doctor doesn’t just pick a drug - they use tools to match you to the right one. First, they check your CHA₂DS₂-VASc score. That’s a point system based on age, sex, heart failure, high blood pressure, diabetes, prior stroke, and vascular disease. If your score is 2 or higher, you’re at high risk for stroke and should be on an anticoagulant.
Then they check your bleeding risk with the HAS-BLED score. Points for high blood pressure, liver or kidney disease, stroke history, lab abnormalities, age over 65, drugs like aspirin, and alcohol use. A score of 3 or higher doesn’t mean you can’t take a blood thinner - it just means you need extra care.
Here’s how most clinicians decide:
- If you’re over 75, have kidney trouble, or weigh less than 60 kg - apixaban is usually best. It’s the safest for frail patients.
- If you want once-daily dosing and have good kidney function - rivaroxaban works well.
- If you’re younger, healthy, and want the most proven stroke prevention - dabigatran is strong, but watch for stomach issues.
- If you have a mechanical valve, severe kidney failure, or take drugs that interact badly with DOACs - stick with warfarin.
What About Side Effects?
All anticoagulants can cause bleeding. But the risk isn’t the same. DOACs cause less brain bleeding. Warfarin causes more. That’s huge - brain bleeds are often fatal or disabling.
Stomach bleeding is more common with dabigatran. If you have a history of ulcers or GERD, apixaban or rivaroxaban might be better. Nosebleeds, bruising, and heavy periods are possible with all of them. The key is knowing when to call your doctor: if you’re bleeding for more than 10 minutes, have blood in your stool or urine, get a severe headache, or fall hard on your head - get help immediately.
There are reversal agents now. Idarucizumab reverses dabigatran. Andexanet alfa reverses apixaban and rivaroxaban. Warfarin can be reversed with vitamin K and fresh plasma. That’s why, in emergencies, warfarin still has an edge - you can undo it fast.
Real-Life Stories
One patient in Melbourne, 79, switched from warfarin to apixaban after 12 years. She used to avoid spinach, broccoli, and green tea. She went to the clinic every month. After switching, she said: “I don’t think about it anymore. I take my pill, I eat what I want, and I sleep better.”
Another, 68, chose warfarin because his Medicare plan covered it fully. He uses a home INR monitor. He checks his blood every two weeks. He says it’s a hassle, but he’s had no strokes or bleeds in 8 years.
On Reddit, one user wrote: “I was on rivaroxaban and had a GI bleed. Switched to apixaban - zero issues since. My GI doc said it’s the safest DOAC.”
What’s Next?
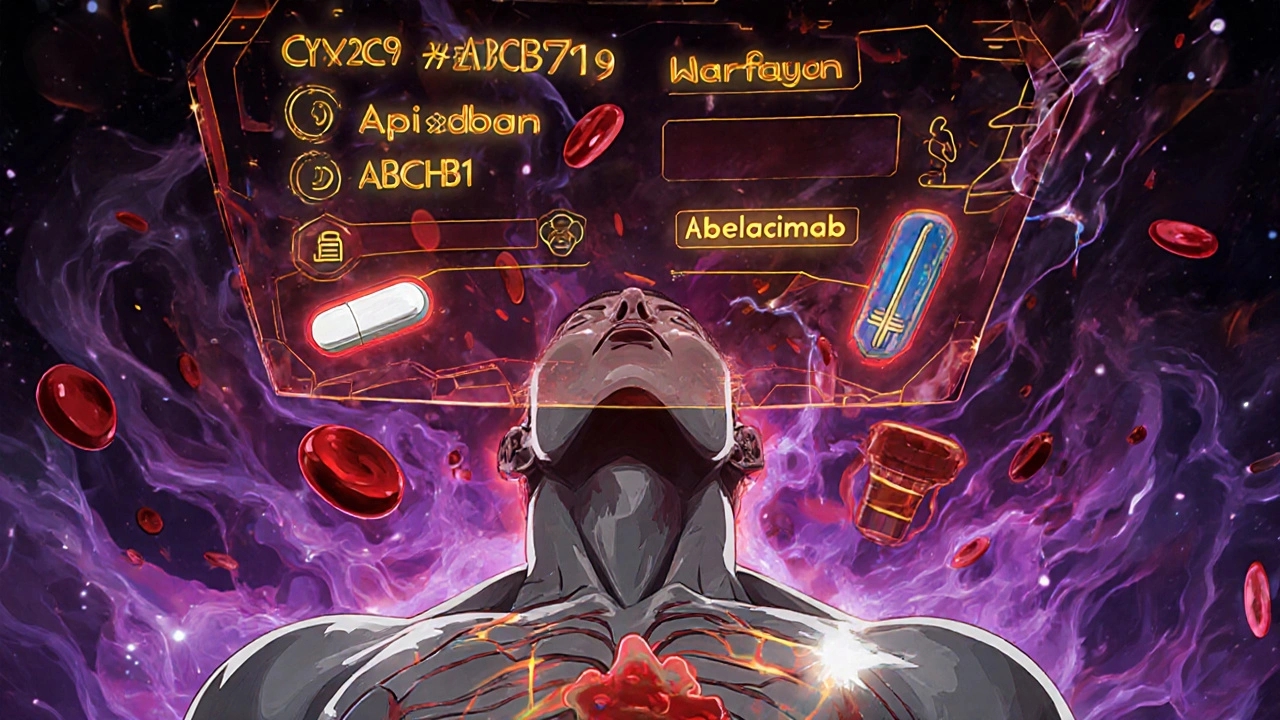
The future is getting smarter. New drugs like milvexian and abelacimab are in trials. They target different parts of the clotting system and promise even lower bleeding risk. One early study showed abelacimab cut major bleeding by 48% compared to apixaban.
Soon, genetic testing may guide your choice. Some people metabolize warfarin slowly because of CYP2C9 gene variants. Others absorb DOACs poorly due to ABCB1 mutations. In five years, your doctor might order a simple DNA test before prescribing.
For now, the message is clear: if you have atrial fibrillation and are at risk for stroke, you need an anticoagulant. DOACs are better for most people - safer, easier, and just as effective. But warfarin still saves lives in specific cases. The right choice isn’t about being modern or old-fashioned - it’s about matching your body, your lifestyle, and your risks.
Are blood thinners the same as antiplatelets like aspirin?
No. Antiplatelets like aspirin stop platelets from clumping. Blood thinners (anticoagulants) stop the clotting cascade proteins. Aspirin reduces stroke risk in atrial fibrillation by only about 20%. Anticoagulants reduce it by 60-70%. For AFib, aspirin is not recommended as a substitute for anticoagulants.
Can I drink alcohol while on blood thinners?
Moderate alcohol is usually okay - one drink a day for women, two for men. But heavy drinking increases bleeding risk, especially with warfarin. Alcohol can also interfere with how your liver processes DOACs. If you drink regularly, tell your doctor. They may adjust your dose or recommend switching.
Do I need to stop blood thinners before surgery?
Sometimes. For minor procedures like dental work, you usually keep taking them. For major surgery, your doctor will decide based on your stroke risk and bleeding risk. DOACs are often stopped 24-48 hours before surgery. Warfarin may be stopped 5 days out, with bridging using heparin if your stroke risk is high. Never stop on your own.
What if I miss a dose?
If you miss a DOAC dose and remember within 6 hours, take it. If it’s more than 6 hours past, skip it and take your next dose at the regular time. Never double up. For warfarin, if you miss a dose, call your clinic - they’ll advise based on your INR. Missing doses increases your stroke risk, so set phone reminders.
How long do I need to take blood thinners?
For atrial fibrillation, it’s usually lifelong. Even if your heart rhythm returns to normal, the risk of clots remains. Stopping increases stroke risk by 5-7% per year. Exceptions include temporary AFib after heart surgery - in those cases, you may stop after 4-6 weeks. Always follow your doctor’s advice.
Final Thoughts
There’s no one-size-fits-all blood thinner. But the data is clear: for most people with atrial fibrillation, DOACs are the better choice. They’re safer, simpler, and more effective than warfarin. The cost gap has closed. The monitoring burden is gone. And the evidence keeps growing.
If you’re on warfarin and tired of blood tests and broccoli restrictions, talk to your doctor about switching. If you’re just starting, ask about apixaban or rivaroxaban. And if you have a mechanical valve or severe kidney disease - don’t assume DOACs are right for you. Work with your team. Your brain is worth the effort.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.