C. difficile Symptom Checker
This tool helps you determine if your symptoms require immediate medical attention after taking clindamycin.
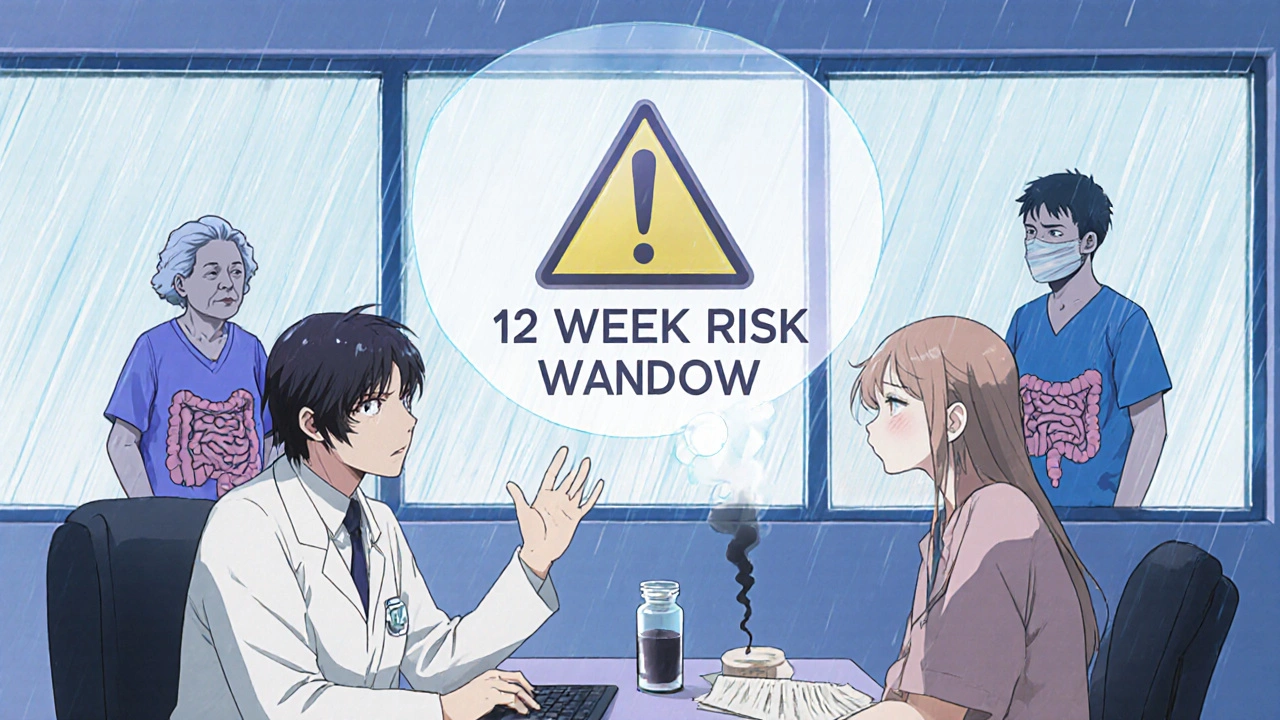
Based on CDC guidelines and recent studies, this assessment checks for symptoms of C. difficile infection that may develop up to 12 weeks after stopping clindamycin. Remember: early treatment reduces complications by over 60%.
Symptom Assessment
Risk Assessment
When you take clindamycin for a tooth infection, skin rash, or other bacterial issue, you’re not just fighting one bug-you’re shaking up your entire gut ecosystem. Clindamycin is powerful, but it’s also one of the riskiest antibiotics out there when it comes to triggering C. difficile infection. This isn’t just a case of mild stomach upset. It’s a potentially life-threatening condition that can turn a simple course of pills into a hospital emergency.
Why Clindamycin Is Different
Not all antibiotics are created equal when it comes to gut damage. Clindamycin stands out because it wipes out a wide range of good bacteria that normally keep Clostridioides difficile in check. While other antibiotics like amoxicillin or doxycycline might cause some disruption, clindamycin is like a sledgehammer to your microbiome. A 2019 study of over 150,000 patients found it carried the highest risk of causing C. difficile infection among all commonly prescribed antibiotics. Even a single dose-like one given before dental work-can be enough to trigger it in some people.The reason? Clindamycin targets gram-positive bacteria, which includes many of the friendly microbes that live in your colon. When those are gone, C. difficile-often already lurking in your gut in small numbers-spreads unchecked. It starts producing toxins that eat away at your intestinal lining, leading to inflammation, severe diarrhea, and sometimes even colon rupture.
When Does C. difficile Show Up?
You might think the danger ends when you finish your last pill. It doesn’t. The window for developing C. difficile infection stretches from the first day you start clindamycin all the way to 12 weeks after you stop. Most cases show up within 5 to 10 days of starting the drug, but 46% happen within a week of finishing the course. That means you can’t just relax after day 7.Some people get sick while still on the antibiotic. Others feel fine for days or even weeks after stopping, then suddenly develop symptoms. That delay is why so many patients dismiss early warning signs. They think, “I’m not on the medicine anymore, so it can’t be that.” But C. difficile doesn’t care when you stopped the pill-it only cares that the gut environment is wide open for it to take over.
What Symptoms Should You Watch For?
The most obvious sign is diarrhea-but not just any diarrhea. You’re looking for:- Three or more loose or watery stools in a 24-hour period
- Stools that don’t hold their shape-think “takes the shape of the toilet bowl”
- Abdominal cramping or pain that’s worse than normal gas
- Fever above 101.3°F (38.5°C)
- Blood or pus in your stool
- Feeling dizzy, thirsty, or urinating much less than usual (signs of dehydration)
These aren’t “just a stomach bug.” If you’ve taken clindamycin in the past 12 weeks and you’re seeing two or more of these symptoms, especially cramping plus diarrhea, you need to call your doctor today. Waiting 48 hours is too long. Studies show people who delay care beyond 72 hours are more than twice as likely to need surgery or die from complications.

Who’s at Highest Risk?
Not everyone who takes clindamycin gets C. difficile. But some people are far more vulnerable:- People over 65
- Those with weakened immune systems (from cancer treatment, HIV, steroids, etc.)
- Anyone who’s had a C. difficile infection before
- People with kidney disease
- Those on other antibiotics at the same time
If you fit into any of these groups, don’t wait for three loose stools. If you get even two in 24 hours-especially with cramping or fever-reach out to your provider immediately. Early treatment cuts the risk of serious complications by over 60%.
What Happens If You Ignore It?
Left untreated, C. difficile doesn’t just cause discomfort-it can destroy your colon. Severe cases lead to toxic megacolon, where the colon swells dangerously and can burst. Or you might develop sepsis, a body-wide infection that can kill in hours. The mortality rate for these advanced cases? Between 35% and 80% without emergency surgery.Even if you survive, you’re at high risk for recurrence. About 1 in 4 people who get C. difficile once will get it again. And each recurrence gets harder to treat. That’s why catching it early isn’t just about feeling better-it’s about staying alive.
What Should You Do If You Suspect C. difficile?
Don’t try to treat it yourself with over-the-counter anti-diarrhea meds like loperamide. Those can trap the toxin inside your body and make things worse. Instead:- Stop taking clindamycin (unless your doctor tells you to keep going-rare, but possible in life-threatening infections)
- Call your doctor or go to an urgent care clinic right away
- Be ready to say: “I took clindamycin in the last 12 weeks and now I have diarrhea, cramps, and [fever/blood/pus].”
- They’ll likely order a stool test for C. difficile toxin
- If confirmed, you’ll be started on an antibiotic like vancomycin or fidaxomicin-both are more effective than older options like metronidazole
In severe cases, you may need to be hospitalized. New treatments like VOWST-a pill made of frozen, purified bacterial spores-are now available to prevent recurrence after the first infection. It’s not a cure, but it’s a major step forward in stopping the cycle.
How to Avoid This in the Future
The best way to avoid C. difficile is to avoid unnecessary antibiotics altogether. Ask your doctor: “Is this really needed? Is there a safer alternative?” For skin infections, trimethoprim-sulfamethoxazole is often just as effective as clindamycin-and much less likely to trigger C. difficile. For dental infections, amoxicillin is usually preferred unless you’re allergic to penicillin.Since 2022, the FDA requires all antibiotic labels to list C. difficile risk. Clindamycin’s label now says it’s in the “highest risk” category. That’s not just fine print-it’s a warning you should take seriously.
Final Thoughts
Clindamycin saves lives. But it can also end them if you don’t pay attention. The risk isn’t huge for every single person-about 1 to 2% of those who take it will get C. difficile. But when it hits, it hits hard. And the window to act is narrow.If you’re on clindamycin-or just finished it-know the signs. Don’t wait for it to get worse. Don’t assume it’s just a stomach bug. If you have diarrhea plus cramps, fever, or blood in your stool, pick up the phone. Your gut is counting on you to act fast.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.