When you’re stuck in a loop of negative thoughts-worrying about what others think, replaying mistakes over and over, or feeling like nothing will ever get better-you’re not just being ‘too sensitive.’ Your brain is operating on outdated software. That’s where cognitive behavioral therapy comes in. It’s not magic. It’s not vague talk about childhoods. It’s a practical, science-backed way to rewire how you think and act, right now.
What Exactly Is Cognitive Behavioral Therapy?
Cognitive Behavioral Therapy, or CBT, is a type of talk therapy built on one simple idea: your thoughts, feelings, and behaviors are connected. Change one, and the others start to shift. It wasn’t always this way. Before the 1960s, most therapy focused on digging up past trauma or unconscious drives. Then psychiatrist Aaron T. Beck noticed something unusual. His patients with depression weren’t just sad-they were convinced they were failures, the world was against them, and the future was hopeless. These weren’t just moods. They were distorted thoughts. Beck called them “automatic negative thoughts.” And he realized: if you can change those thoughts, you can change how you feel. CBT combines two parts: cognitive (how you think) and behavioral (what you do). It’s not about feeling better by talking endlessly. It’s about learning skills. Like how to spot when your brain is lying to you, or how to face fears instead of avoiding them. The goal? To give you tools you can use long after therapy ends.Why Is CBT Called the Gold Standard?
More than 2,000 clinical studies have tested CBT. That’s more than any other form of therapy. The results? Consistent. Powerful. The National Institute for Health and Care Excellence (NICE) in the UK has listed CBT as the first-choice treatment for depression, anxiety, PTSD, OCD, and eating disorders since 2004. The American Psychological Association says the same. Why? Because it works-and it works fast. For example, in a major study published in JAMA Psychiatry, people with depression who did CBT had a 52% chance of staying well after 12 months. Those on antidepressants alone? Only 47%. And here’s the kicker: the CBT group had less than half the relapse rate. That’s not a small difference. That’s life-changing. CBT also beats other therapies in head-to-head comparisons. For anxiety disorders, CBT’s effectiveness is about 30% higher than traditional talk therapy. For panic attacks, it reduces them by 70-80% in just 12 sessions. And unlike medication, the benefits stick. You’re not dependent on pills. You’re equipped with skills.How Does CBT Actually Work in Practice?
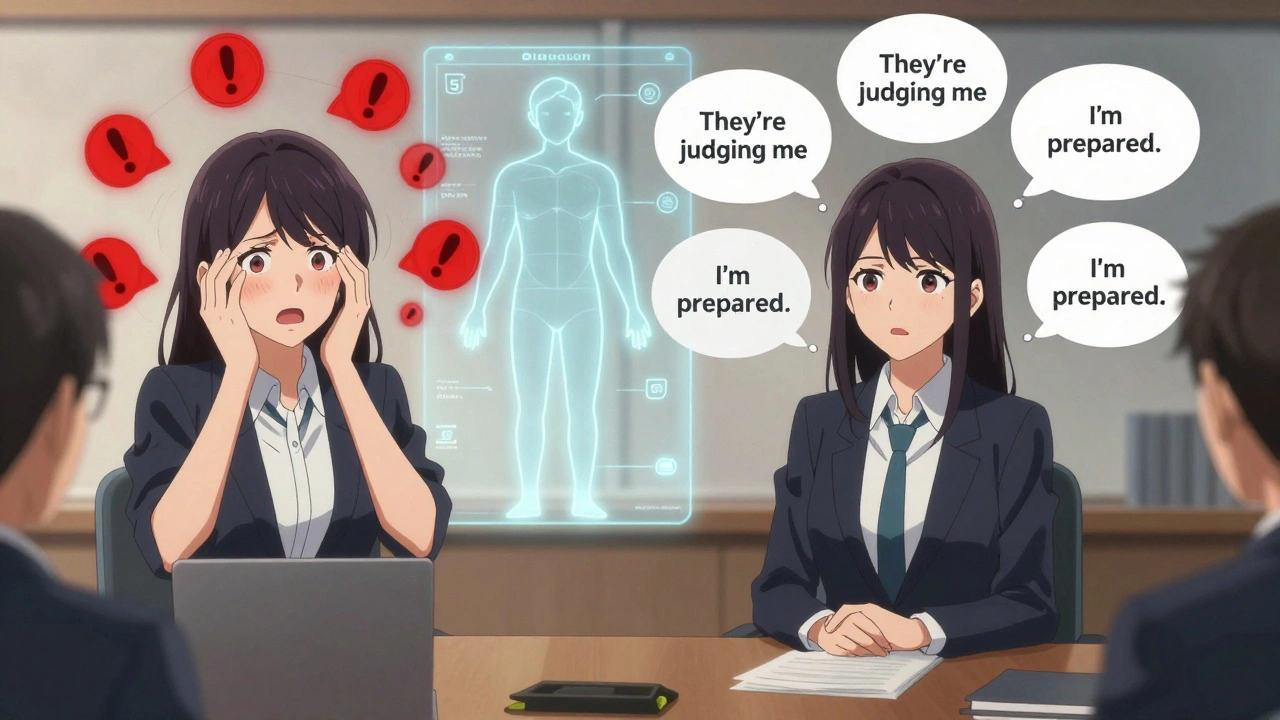
Most CBT sessions last 45 to 60 minutes and happen once a week for 8 to 20 weeks. It’s not open-ended. You don’t stay in therapy for years. You learn, you practice, you move on. Here’s what happens in a typical session:- You identify a problem: “I panic before meetings.”
- You track your thoughts: “If I mess up, everyone will think I’m incompetent.”
- You challenge those thoughts: “Have I ever seen someone else mess up and get fired? No. Most people don’t even notice.”
- You test it out: You volunteer to speak up in a small team meeting-and realize nothing bad happens.
- You do homework: You write down your thoughts and reactions daily. It’s like journaling, but with a purpose.
What Conditions Does CBT Actually Help?
CBT isn’t a one-size-fits-all fix. But it’s been proven effective for a wide range of issues:- Depression: Helps break the cycle of hopelessness and inactivity.
- Anxiety disorders (generalized, social, panic): Teaches you to tolerate uncertainty and reduce avoidance.
- PTSD: Uses exposure techniques to reduce the power of traumatic memories.
- OCD: Exposure and Response Prevention (a CBT subtype) stops the compulsive cycle.
- Eating disorders: Addresses distorted body image and rigid food rules.
- Insomnia: Targets the racing thoughts and bedtime rituals that keep you awake.
- Chronic pain: Helps manage the emotional toll and fear of movement.
- Substance use: Builds coping skills to replace drug use with healthier behaviors.
What Are the Limits of CBT?
CBT isn’t perfect. And it’s not for everyone. For people with severe trauma, complex PTSD, or borderline personality disorder, therapies like Dialectical Behavior Therapy (DBT) often work better. DBT adds emotion regulation and mindfulness, which CBT doesn’t always focus on. CBT also requires effort. You have to do homework. You have to sit with discomfort during exposure exercises. Some people quit because it’s hard. In fact, about 32% of negative reviews mention the homework as too demanding. If you’re feeling too overwhelmed to write a single thought record, CBT might feel like another burden. It’s also not ideal for people with severe cognitive impairment, active psychosis, or very low motivation. You need some ability to reflect, analyze, and follow through. That’s not a flaw in CBT-it’s just a limitation of how it’s designed.CBT vs. Other Therapies: What’s the Difference?
Let’s compare CBT to a few other common approaches:| Therapy Type | Focus | Duration | Homework? | Best For |
|---|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Thoughts, behaviors, present problems | 8-20 weeks | Yes | Anxiety, depression, OCD, PTSD |
| Psychodynamic Therapy | Unconscious patterns, childhood experiences | 1-5 years | Rarely | Personality insight, long-standing relationship issues |
| Dialectical Behavior Therapy (DBT) | Emotions, distress tolerance, mindfulness | 6-12 months | Yes | Borderline personality, self-harm, intense emotions |
| Acceptance and Commitment Therapy (ACT) | Accepting thoughts, values-based action | 12-20 weeks | Yes | Chronic pain, stress, perfectionism |
| Medication (e.g., SSRIs) | Brain chemistry | Months to years | No | Severe depression, acute anxiety |
Real People, Real Results
On Reddit’s r/mentalhealth, thousands of people share their CBT stories. One user wrote: “I had 15 panic attacks a week. After 10 sessions of graded exposure, I had two. Then none.” Another said: “I used to avoid parties because I thought everyone was judging me. I did a ‘behavioral experiment’-I went, said hi to three people, and no one stared. My brain finally got the message.” A case study in the Journal of Clinical Psychology followed a woman with severe OCD. She spent hours washing her hands and checking locks. After 18 sessions of Exposure and Response Prevention (a CBT technique), she stopped all compulsions. She went back to work. She started dating again. That’s not just symptom reduction. That’s life restoration.Can You Do CBT on Your Own?
Yes-and many people do. There are free CBT workbooks from the National Alliance on Mental Illness (NAMI), apps like Woebot (FDA-cleared), and online programs backed by the NHS. But here’s the catch: self-guided CBT works best for mild to moderate symptoms. For severe depression, trauma, or suicidal thoughts, working with a trained therapist is critical. Therapists aren’t just guides-they’re accountability partners. They catch when you’re avoiding, when your thoughts are distorted, or when you’re stuck. They adjust the plan. They help you push through the hard parts.
How to Find a CBT Therapist
In the UK, you can get CBT through the NHS via IAPT (Improving Access to Psychological Therapies) services. Wait times vary, but it’s free. If you’re paying privately, look for therapists certified by the British Association for Behavioural and Cognitive Psychotherapies (BABCP) or the Academy of Cognitive Therapy. Ask: “Are you trained in CBT?” “Do you use structured treatment manuals?” “Will I get homework?” If they say, “We’ll just talk about your childhood,” they’re not doing CBT.What’s Next for CBT?
CBT isn’t stuck in the past. New versions are emerging. Third-wave CBT-like ACT and Mindfulness-Based Cognitive Therapy-adds acceptance and mindfulness. AI tools are being developed to analyze thought records in real time. Researchers are even exploring how to match CBT techniques to brain activity patterns. But the core hasn’t changed: your thoughts shape your reality. And you can learn to change them.Frequently Asked Questions
Is CBT just positive thinking?
No. CBT isn’t about forcing yourself to think happy thoughts. It’s about spotting when your thoughts are inaccurate, exaggerated, or unhelpful-and replacing them with ones that are more realistic. For example, instead of thinking, “I’ll never get better,” you might learn to say, “I’m having a hard time right now, but I’ve improved before, and I can use these skills again.” It’s not about being positive. It’s about being accurate.
How long until I feel better with CBT?
Most people start noticing changes in 4 to 6 weeks. For anxiety or mild depression, many see major improvement by week 8 to 12. But it’s not instant. You’re rewiring habits built over years. It takes practice. Think of it like going to the gym-you don’t get stronger after one session. But after 8 weeks of consistent work, you’ll notice a difference.
Does CBT work for everyone?
Not everyone. People with severe cognitive impairment, active psychosis, or very low motivation often struggle with the structure and homework. CBT also doesn’t focus much on deep emotional wounds from childhood, so if your main issue is unresolved trauma, therapies like EMDR or DBT might be better. But for anxiety, depression, OCD, and PTSD? CBT is the most reliable option we have.
Can I use CBT alongside medication?
Yes, and many people do. In fact, studies show that combining CBT with antidepressants works better than either alone for moderate to severe depression. Medication can help stabilize your mood enough to engage in therapy. Therapy helps prevent relapse once you stop the meds. They’re not competing-they’re complementary.
What if I hate homework?
It’s common. Homework is one of the biggest reasons people drop out. But therapists can adjust. Start small: write down just one thought per day. Or do a behavioral experiment-like making one phone call you’ve been avoiding. The goal isn’t perfection. It’s progress. Even 10 minutes a day builds momentum. And if you’re truly overwhelmed, tell your therapist. They’ll help you scale back, not quit.
Next Steps
If you’re considering CBT:- Try a free CBT workbook from NAMI or the NHS website.
- Ask your GP for a referral to IAPT if you’re in the UK.
- If paying privately, check BABCP’s directory for certified therapists.
- Be ready to do the work. Therapy isn’t passive.
- Give it at least 8 weeks before deciding if it’s right for you.


I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.