HIV Treatment Comparison Tool
Compare Your HIV Treatment Options
Select your current treatment and priorities to see how modern alternatives compare in effectiveness, side effects, cost, and convenience.
Your Current Treatment
Your Priorities
Select the factors most important to you when choosing treatment:
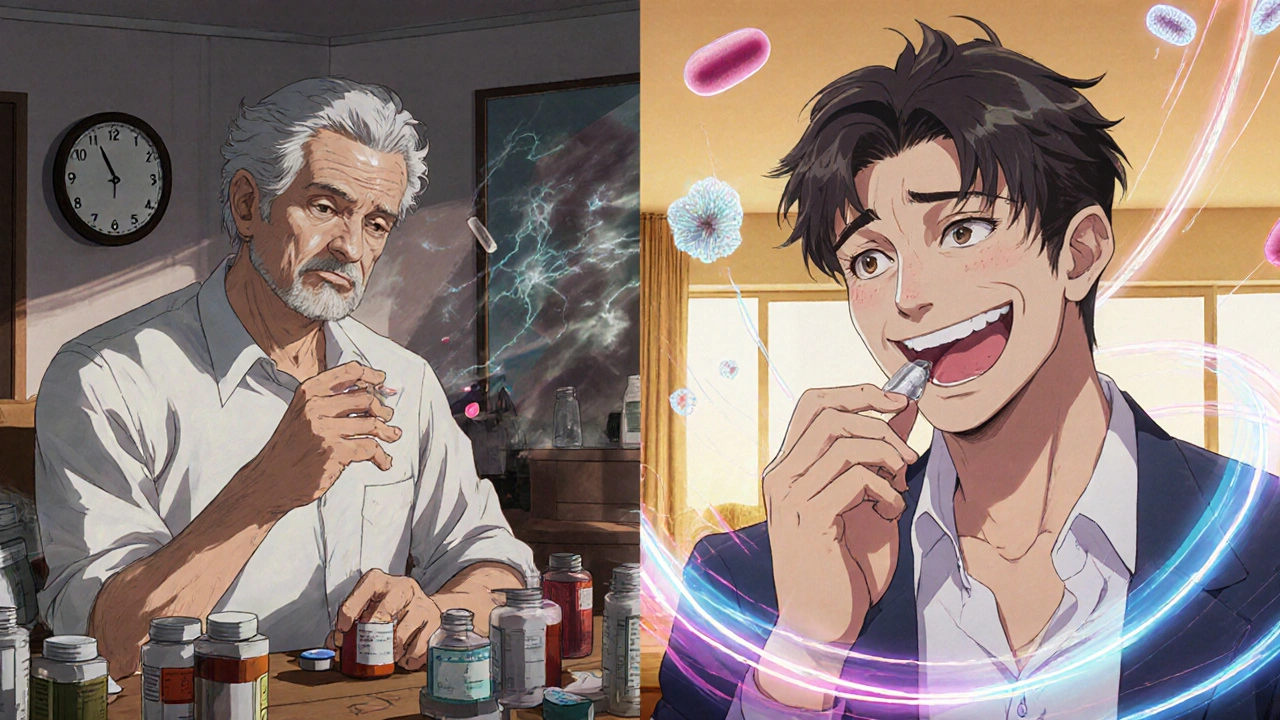
Combivir was once a backbone of HIV treatment - a single pill combining lamivudine and zidovudine, two of the first antiretrovirals approved to fight HIV. But today, it’s rarely prescribed in places like Australia, the U.S., or Europe. Why? Because better options exist. If you’re still on Combivir, or you’re researching it for yourself or someone else, you’re not alone. Many people are wondering: is there something safer, simpler, or more effective?
What Combivir Actually Does
Combivir is a fixed-dose combination of two nucleoside reverse transcriptase inhibitors (NRTIs): Lamivudine and a nucleoside analog that blocks HIV from copying its genetic material, and Zidovudine a similar drug that interferes with HIV replication. Together, they were designed to reduce the viral load - the amount of HIV in the blood - and slow disease progression.
When Combivir came out in the late 1990s, it was a breakthrough. Before that, patients had to take multiple pills at different times of day. Combivir cut that in half. But its side effects were serious: anemia, muscle weakness, nerve damage, and a rare but dangerous buildup of lactic acid in the blood. Long-term use also raised the risk of fat loss in the face and limbs, a condition called lipodystrophy.
Why Combivir Is No Longer First-Line
By 2010, guidelines from the World Health Organization and the U.S. Department of Health and Human Services stopped recommending Combivir as a starting treatment. Why? Three reasons:
- Higher toxicity - Zidovudine causes bone marrow suppression more often than newer drugs.
- Lower barrier to resistance - HIV mutates more easily around lamivudine and zidovudine than around drugs like tenofovir or dolutegravir.
- Better alternatives - Modern pills combine fewer side effects with higher effectiveness.
Studies from the Journal of Infectious Diseases in 2022 showed that patients switched from Combivir to newer regimens had a 40% lower risk of developing drug resistance and 30% fewer treatment interruptions due to side effects.
Top Modern Alternatives to Combivir
Today, most people with HIV start on a single pill that contains three drugs - two NRTIs plus an integrase inhibitor. These regimens are easier, safer, and more effective. Here are the most common alternatives:
| Regimen | Active Ingredients | Dosing | Side Effect Profile | Resistance Barrier |
|---|---|---|---|---|
| Combivir | Lamivudine, Zidovudine | Twice daily | High: anemia, fatigue, neuropathy | Low |
| Descovy | Emtricitabine, Tenofovir alafenamide | Once daily | Low: mild nausea, rare kidney issues | High |
| Truvada | Emtricitabine, Tenofovir disoproxil fumarate | Once daily | Moderate: possible bone density loss | High |
| Biktarvy | Bictegravir, Emtricitabine, Tenofovir alafenamide | Once daily | Very low: rarely causes side effects | Very high |
| Dovato | Dolutegravir, Lamivudine | Once daily | Low: headache, insomnia | High |
Notice something? Most modern regimens replace zidovudine with tenofovir or emtricitabine - drugs with far fewer long-term risks. Biktarvy and Dovato are now the most popular first-choice regimens in Australia and the U.S. because they’re single pills, taken once a day, and rarely cause problems.

When Might Someone Still Be on Combivir?
Even though it’s outdated, some people still take Combivir. Why?
- Cost - In some low-income countries, Combivir is cheaper than newer drugs.
- Access - In rural clinics or underfunded health systems, newer meds aren’t always available.
- History - Some patients started on Combivir decades ago and haven’t switched because they’re stable.
But stability doesn’t mean safety. A 2023 study in The Lancet HIV followed 1,200 patients on older NRTI combinations like Combivir. After five years, 18% developed moderate to severe anemia, and 12% showed signs of mitochondrial toxicity - damage that can affect the liver, nerves, and muscles.
If you’re on Combivir and feel fine, don’t assume you’re in the clear. Regular blood tests for hemoglobin, lactate, and liver enzymes are critical. If those numbers start drifting, switching isn’t just a good idea - it’s necessary.
Switching from Combivir: What to Expect
Switching from Combivir to a modern regimen is usually straightforward. Doctors don’t usually need to stop your current meds before starting the new one. Most transitions happen over a few days.
Here’s what typically happens:
- Your doctor checks your viral load and CD4 count to make sure your HIV is well-controlled.
- They test your kidney and liver function - especially if you’ve been on zidovudine for years.
- They pick a new regimen based on your history, resistance tests, and any other health conditions.
- You start the new pill, often the same day or the next.
- You return in 4-6 weeks for a follow-up viral load test to confirm the new drug is working.
Most people report feeling better within weeks: more energy, fewer aches, better sleep. One patient in Melbourne, 58, switched from Combivir to Biktarvy in early 2024. He said, "I stopped needing naps after lunch. My hands stopped tingling. I felt like I was 40 again."
What About Cost and Insurance?
In Australia, Combivir is no longer subsidized under the Pharmaceutical Benefits Scheme (PBS). That means you’d pay full price - around $150 per month - for a drug that’s outdated and riskier than alternatives.
Modern regimens like Biktarvy and Dovato are PBS-subsidized. That means you pay the standard co-payment: about $31.10 for concession card holders, $30.50 for general patients. Even if you’re paying out of pocket, newer drugs often cost less than Combivir because they’re more widely produced and used.
Insurance in the U.S. and Canada also covers modern regimens almost universally. Combivir is rarely covered unless you have a documented allergy or intolerance to all alternatives - and even then, it’s a last resort.
What You Should Do Next
If you’re on Combivir:
- Don’t stop taking it suddenly. That can cause your viral load to spike.
- Ask your doctor for a resistance test if you haven’t had one in the last year.
- Request a full blood panel - check hemoglobin, lactate, and liver enzymes.
- Ask: "Is there a simpler, safer pill I could switch to?"
If you’re considering starting HIV treatment:
- Never start with Combivir. It’s not recommended anywhere in the developed world.
- Ask for a single-pill regimen like Biktarvy, Dovato, or Descovy + dolutegravir.
- Make sure your provider checks for kidney function and bone health before prescribing.
Frequently Asked Questions
Is Combivir still available anywhere?
Yes, but mostly in low- and middle-income countries where newer drugs are too expensive or hard to distribute. In Australia, the U.S., Canada, and the EU, Combivir is no longer routinely stocked by pharmacies. It’s only available through special orders, and even then, doctors rarely prescribe it.
Can I switch from Combivir to a newer drug if I’ve been on it for years?
Absolutely. Many people switch successfully after 10, 15, or even 20 years on Combivir. The key is doing it under medical supervision. Your doctor will check your viral load, resistance profile, and organ function before switching. Most transitions are smooth, with no rebound in virus levels.
Why is zidovudine considered risky long-term?
Zidovudine can suppress bone marrow, leading to low red blood cells (anemia), low white blood cells (neutropenia), and muscle damage. It also causes mitochondrial toxicity - damage to the energy-producing parts of your cells. Over time, this can lead to nerve pain, liver problems, and unusual fat loss. Newer drugs like tenofovir alafenamide don’t carry these risks.
Are there any side effects with modern HIV drugs?
Modern drugs like Biktarvy and Dovato are among the safest HIV treatments ever made. Most people have no side effects. The most common are mild headaches, nausea, or trouble sleeping - and these usually fade within weeks. Serious side effects are extremely rare. This is why they’re now first-line choices worldwide.
Can I get help paying for a new HIV medication?
In Australia, the PBS covers most modern HIV regimens, so you pay only the standard co-payment. In the U.S., patient assistance programs from drug manufacturers (like Gilead’s Advancing Access) can reduce or eliminate out-of-pocket costs. Nonprofits like the AIDS Drug Assistance Program (ADAP) also help eligible patients. Always ask your clinic’s social worker - they’re trained to help with this.
Final Thoughts
Combivir helped save lives in the 90s and early 2000s. But medicine doesn’t stand still. Today’s HIV treatments are simpler, safer, and more effective than ever. Staying on Combivir isn’t a badge of loyalty - it’s a missed opportunity for better health.
If you’re on it, talk to your doctor. If you’re not, make sure you’re not starting with it. The goal isn’t just to control HIV - it’s to live well with it. And modern medicine makes that possible for nearly everyone.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.