Dry Mouth Severity Assessment
This assessment will help you determine the severity of your dry mouth and provide personalized recommendations based on your symptoms.
Your Dry Mouth Severity Level
Recommended Strategies
Key Takeaways
- Radiation, chemotherapy, and immunotherapy can damage salivary glands, leading to xerostomia.
- Staying hydrated, using gentle oral care products, and chewing sugar‑free gum are quick wins.
- Prescription sialogogues such as pilocarpine or cevimeline boost saliva production for many patients.
- Over‑the‑counter saliva substitutes and natural moisturizers provide short‑term comfort.
- Regular check‑ins with your oncology and dental teams prevent infections and protect quality of life.
Xerostomia is the medical term for dry mouth. It occurs when the salivary glands don’t make enough saliva, leaving the mouth feeling parched, sticky, and sometimes painful.
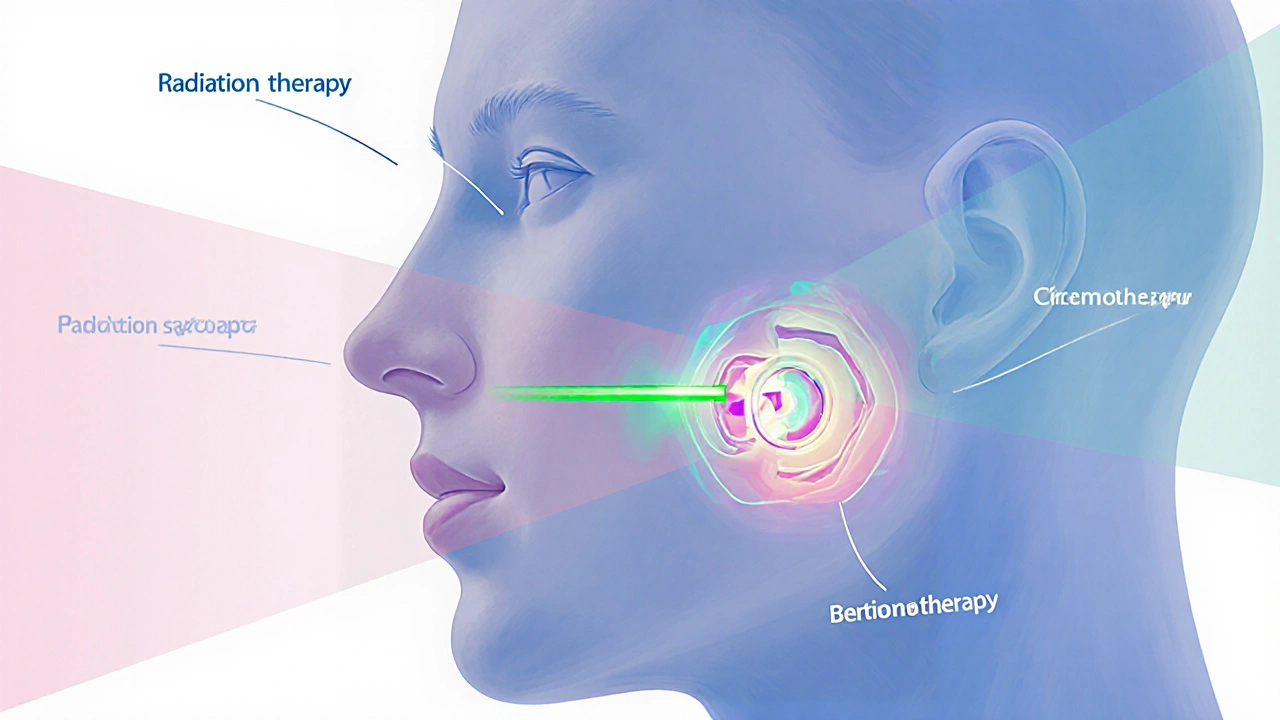
Why Cancer Treatments Trigger Dry Mouth
Three major cancer therapies can interfere with saliva production:
- Radiation therapy is a treatment that uses high‑energy beams to kill cancer cells. When the head or neck area receives radiation, the salivary glands absorb a dose of radiation and may become inflamed or permanently damaged.
- Chemotherapy circulates throughout the body, targeting rapidly dividing cells. Some drugs, especially antimetabolites and alkylating agents, reduce saliva output by affecting the glandular tissue.
- Immunotherapy boosts the immune system to attack cancer. Certain checkpoint inhibitors can trigger inflammatory reactions in the mouth, indirectly reducing saliva flow.
The common denominator is damage to the salivary glands, the organs that churn out the watery fluid that keeps your mouth moist, washes away bacteria, and starts digestion.
How Dry Mouth Impacts Daily Life
When saliva thins out, you may notice:
- A burning or gritty sensation in the tongue and palate.
- Difficulty swallowing solid foods or even liquids.
- Increased thirst and the urge to sip water constantly.
- Changes in taste - foods may taste bland or metallic.
- Higher risk of cavities, fungal infections, and oral mucositis, a painful inflammation of the mouth lining.
All these symptoms can erode confidence, affect nutrition, and lower quality of life during an already stressful treatment period.
Immediate Self‑Care Steps
Before reaching for any product, try these low‑effort habits:
- Sip, don’t gulp. Take small sips of room‑temperature water every 15‑20 minutes.
- Choose a soft toothbrush. Brush gently twice a day with a fluoride toothpaste to keep plaque at bay without irritating sensitive tissue.
- Rinse with a mild, alcohol‑free mouthwash. Look for formulas containing xylitol or aloe vera, which soothe without drying.
- Chew sugar‑free gum or suck on lozenges. The act of chewing stimulates whatever saliva the glands can still produce.
- Adjust your diet. Favor moist foods-soups, stews, oatmeal, and yoghurt. Avoid salty, dry, or overly spicy items that can exacerbate dryness.

Prescription‑Level Relief: Sialogogues
If home measures aren’t enough, talk to your oncologist about medications that actively increase saliva flow. Two commonly prescribed options are:
- Pilocarpine is an oral cholinergic agonist that binds to receptors in the salivary glands, prompting them to secrete more fluid.
- Typical dose: 5 mg three times daily. Side effects may include sweating, nausea, or increased urinary frequency.
- Cevimeline works similarly but tends to cause fewer gastrointestinal symptoms.
- Typical dose: 30 mg three times daily. Watch for headache or dizziness.
Both drugs belong to the broader class of sialogogues, agents that stimulate saliva production. They’re most effective when taken before meals or before a nighttime sleep period.
Over‑The‑Counter and Natural Aids
When prescriptions aren’t suitable, these options can still bring noticeable comfort:
- Saliva substitutes. Sprays, gels, and lozenges that mimic the lubricating properties of natural saliva. Look for products containing carboxymethylcellulose or hydroxyethylcellulose.
- Humidifiers. Running a cool‑mist humidifier in your bedroom adds moisture to the air, reducing nighttime dryness.
- Honey or maple syrup. A teaspoon of a natural sweetener can coat the oral mucosa temporarily. Use sparingly if you’re diabetic.
- Green tea rinse. Cool brewed tea (unsweetened) swished for 30 seconds can soothe irritation and add a mild antioxidant boost.
Medical Comparison: What Works Best?
| Option | How it works | Typical onset | Pros | Cons |
|---|---|---|---|---|
| Prescription sialogogues (pilocarpine, cevimeline) | Stimulates salivary gland receptors | 30‑60 minutes | Long‑lasting increase in natural saliva | Possible systemic side effects; requires doctor approval |
| Saliva substitutes (sprays, gels) | Provides external lubrication | Immediate | Easy to use; no prescription needed | Temporary; may need frequent re‑application |
| Chewing sugar‑free gum / lozenges | Triggers residual gland activity | 5‑10 minutes | Inexpensive; also freshens breath | Limited effect if glands are severely damaged |
| Humidifier + water intake | Increases ambient moisture and hydration | Continuous | Improves overall comfort; no medication | Requires equipment; may not address oral dryness directly |
When to Seek Professional Help
Even with diligent self‑care, certain signs warrant a visit to your oncology or dental team:
- Persistent burning or ulceration that doesn’t heal within two weeks.
- Repeated cavities despite flossing and fluoride use.
- Unexplained weight loss due to difficulty swallowing.
- Frequent oral infections, such as thrush (candida).
Your dental hygienist can provide targeted fluoride treatments and recommend customized mouth rinses that are safe during cancer therapy. The oncologist can adjust radiation fields or prescribe sialogogues as part of a supportive‑care plan.

Preventing Complications
Dry mouth isn’t just uncomfortable-it can pave the way for serious oral health problems. Follow these safeguards:
- Fluoride daily. Use a 0.05% sodium fluoride rinse or a custom tray if your dentist recommends it.
- Avoid tobacco and alcohol. Both dry out tissues and increase infection risk.
- Schedule regular dental check‑ups. Even if you feel fine, a professional exam catches early decay.
- Keep a symptom diary. Note when dryness spikes (e.g., after a chemo session) to discuss patterns with your care team.
Quick Daily Checklist
- Drink 8‑10 glasses of water spread throughout the day.
- Brush with a soft brush and fluoride toothpaste after meals.
- Chew sugar‑free gum for 5‑10 minutes after eating.
- Apply a saliva substitute before bedtime.
- Run a humidifier while you sleep.
- Record any new sores, taste changes, or increased thirst.
Putting It All Together: Your Personal Relief Plan
Start by assessing the severity of your xerostomia-mild, moderate, or severe. Then layer strategies:
- Base layer: Hydration, oral hygiene, sugar‑free gum.
- Mid layer: Saliva substitutes and a bedside humidifier.
- Top layer (if needed): Prescription sialogogues under doctor supervision.
Adjust each layer as your treatment cycle changes. Remember, the goal is dry mouth relief that lets you eat, talk, and smile without constant discomfort.
Frequently Asked Questions
Can I use over‑the‑counter mouthwash if I’m undergoing radiation?
Yes, but choose an alcohol‑free formula with soothing ingredients like aloe or xylitol. Alcohol can further dry out the mouth and irritate mucosal tissue.
How long does it take for pilocarpine to start working?
Most patients notice increased saliva within 30 to 60 minutes after the first dose. Maximum benefit often appears after a few days of consistent use.
Is it safe to chew gum if I have oral mucositis?
If the mouth is ulcerated, chewing can worsen pain. Wait until lesions heal, then switch to gentle sugar‑free gum.
Should I avoid coffee and tea?
Caffeinated drinks can have a mild diuretic effect, increasing thirst. If you do drink them, pair with water and consider decaf options.
What’s the best way to clean dentures if I have dry mouth?
Remove dentures after meals, rinse with warm water, and soak in a fluoride‑containing soak solution. Avoid mouthwashes containing alcohol.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.