The same pill, different name. You pick up a generic version of your blood pressure medication, cheaper and just as effective-or so you hope. But how does the FDA make sure it actually works like the brand-name version? The answer isn’t in clinical trials with thousands of patients. It’s in a lab, with a machine spinning a basket, dissolving tablets in fluid, and measuring how fast the drug comes out. This is dissolution testing, and it’s the backbone of how the FDA guarantees that generic drugs are safe and effective without repeating expensive human studies.
Why Dissolution Testing Matters
Generic drugs aren’t copies. They’re exact matches in active ingredients, strength, and dosage form. But matching the label isn’t enough. A pill might contain the right amount of drug, but if it doesn’t dissolve the same way in your stomach, it won’t be absorbed the same way. That means it might not work-or worse, it could cause side effects. Dissolution testing measures how quickly and completely a drug releases from its tablet, capsule, or suspension under controlled lab conditions. It’s not a guess. It’s a science-backed predictor of what happens inside your body.The FDA doesn’t require every generic drug to be tested in people. Instead, they use dissolution data as a stand-in. If the generic dissolves at the same rate and extent as the brand-name drug, it’s very likely to behave the same in your bloodstream. This saves time, money, and avoids putting healthy volunteers through unnecessary trials. For the FDA, dissolution testing is the most efficient way to ensure quality without compromising safety.
What the FDA Actually Requires
When a company submits an Abbreviated New Drug Application (ANDA) for a generic, they must include detailed dissolution data in five specific areas. It’s not a checklist-it’s a full scientific dossier.- Solubility of the active ingredient: Is the drug easily dissolved in water or stomach fluid? This determines how hard it is to get it out of the pill.
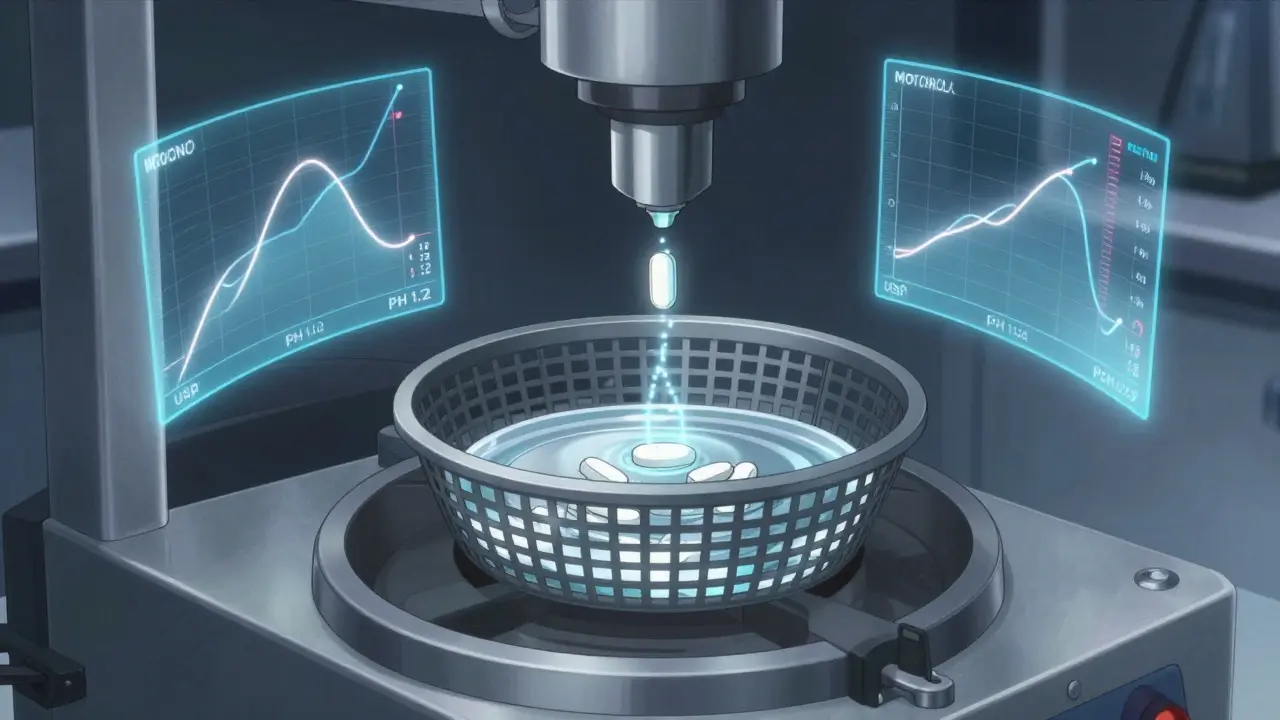
- Test method setup: What machine is used? (Usually USP Apparatus 1 or 2.) What’s the rotation speed? (Typically 50-100 rpm.) What liquid is used? (pH 1.2 for stomach, pH 6.8 for intestines.) How much fluid? (Usually 500-900 mL.) When are samples taken? (Every 5-15 minutes, depending on the drug.)
- Method validation: Has the test been proven to work consistently? Can it handle small changes in temperature, pH, or equipment? If the method breaks under minor stress, it’s not reliable.
- Analytical accuracy: Can the lab accurately measure how much drug is dissolved? This isn’t just about taste-it’s about precise chemical detection, often using high-performance liquid chromatography (HPLC).
- Discriminatory power: Does the test catch differences? For a low-solubility drug, two formulations might look identical on paper but behave very differently in the body. The dissolution test must be sensitive enough to spot those differences.
For immediate-release pills-like most antibiotics or painkillers-the standard is clear: at least 80% of the drug must dissolve within 45 minutes. But this isn’t a one-size-fits-all rule. The FDA tailors the requirement to the drug. For example, if the drug is highly soluble and highly absorbable (BCS Class I), the FDA allows a single-point test: just check at 30 minutes using 900 mL of 0.1N HCl. If the generic matches the brand at that point, it’s approved without needing human bioequivalence studies.
How the FDA Compares Products
It’s not enough for a generic to dissolve 80% in 45 minutes. It has to match the brand-name drug’s entire dissolution profile. That’s where the f2 similarity factor comes in. This is a statistical tool that compares the dissolution curves of the generic and the reference product over time. Think of it like matching two heartbeats-not just the peak, but the rhythm.An f2 score of 50 or higher means the two profiles are similar enough to be considered equivalent. If the score is below 50, the FDA asks for more data. Sometimes, manufacturers have to tweak their formula-change a binder, adjust particle size, or modify the coating-to get the curve to line up. The FDA doesn’t accept a “close enough” answer. They want the curves to match like twins.
Special Cases: Modified-Release and Complex Drugs
Not all pills are made the same. Extended-release tablets are designed to release drug slowly over 8, 12, or even 24 hours. For these, dissolution testing gets much more complicated. The FDA requires testing under multiple pH levels-stomach acid (pH 1.2), small intestine (pH 4.5), and colon (pH 6.8)-to simulate how the drug behaves as it moves through your digestive tract.There’s also alcohol testing. Many extended-release drugs can “dose-dump”-release all their drug at once-if taken with alcohol. The FDA requires manufacturers to test their product with up to 40% ethanol in the dissolution medium. If the drug releases too fast under these conditions, the label must warn against drinking alcohol with it. This isn’t hypothetical. There have been real cases where patients were hospitalized after mixing alcohol with poorly designed generics.
For low-solubility drugs-like many cholesterol or antifungal medications-dissolution testing can take over a year to develop. These drugs don’t dissolve easily, so manufacturers have to use complex methods: surfactants, different buffers, or even biorelevant media that mimic human intestinal fluid. The FDA expects full documentation of every decision made during this process. No shortcuts.
The FDA’s Dissolution Database
You won’t find this on the FDA website unless you’re a scientist, but it’s one of the most powerful tools in generic drug approval: the Dissolution Methods Database. As of late 2023, it contains over 2,800 recommended dissolution methods for specific drug products. If your generic is for a drug already in the database, you don’t start from scratch. You follow the method. This saves companies months of development time and ensures consistency across all generics for that drug.But if your drug isn’t listed? Then you have to develop your own method from scratch. And you have to prove it works. The FDA doesn’t accept methods just because they’re convenient. They must be scientifically justified, validated, and capable of distinguishing between good and bad formulations. This is why some generic manufacturers spend 6-12 months just on dissolution testing before submitting an application.

What Happens After Approval?
Approval isn’t the end. The FDA uses dissolution testing to monitor changes after a drug hits the market. If a company switches suppliers, changes the manufacturing site, or tweaks an excipient, they must prove the dissolution profile hasn’t changed. This is called SUPAC-IR (Scale-Up and Post-Approval Changes for Immediate Release products). If the new version dissolves differently, the FDA can reject the change-or pull the product.There have been cases where manufacturers changed the coating on a tablet to reduce cost, only to find out later that the drug was dissolving too slowly. The FDA flagged it. The product was pulled. Patients were switched back to the original version. Dissolution testing caught it before anyone got sick.
Why This System Works
The FDA’s approach is smart. Instead of testing every generic in people, they use a highly controlled, repeatable lab test that predicts real-world performance. It’s faster, cheaper, and just as reliable-for the right drugs. For BCS Class I drugs, biowaivers (waiving human studies) are now routine. By 2025, an estimated 35% of all generic approvals will use this streamlined path, up from 25% in 2020.But the FDA is careful. They don’t apply this to every drug. Low-solubility drugs? Still require full testing. Modified-release? More conditions. Complex formulations? More data. The agency doesn’t cut corners. It uses science to decide where it can.
Dissolution testing isn’t flashy. No headlines. No celebrity endorsements. But every time you take a generic pill and feel better, it’s because this quiet, meticulous process worked. The FDA didn’t just approve a drug. They approved a promise-that the cheaper version would do exactly what the expensive one did.
Is dissolution testing required for all generic drugs?
No, but it’s required for nearly all oral solid dosage forms-tablets, capsules, and suspensions. Drugs already in solution, like oral liquids or topical creams, are exempt because their active ingredients are already dissolved. The FDA focuses on products where dissolution rate affects absorption.
Can a generic drug be approved even if its dissolution profile doesn’t match the brand?
Rarely, and only under specific circumstances. If the generic performs differently in dissolution but shows bioequivalence in human studies, the FDA may approve it with different dissolution specifications. This happens when the brand’s method isn’t discriminatory enough. But the generic must still prove it’s safe and effective-dissolution is a guide, not the only rule.
What is the f2 similarity factor, and why is it important?
The f2 factor is a statistical measure that compares the dissolution profiles of two drugs over time. An f2 score of 50 or higher means the two curves are similar enough to be considered equivalent. It’s not just about matching one time point-it’s about matching the entire pattern of drug release. This ensures the generic behaves like the brand throughout the absorption window.
Why does the FDA use different pH levels in dissolution testing?
Your stomach and intestines have different pH levels. A drug might dissolve quickly in stomach acid but not in the intestine-or vice versa. Testing at pH 1.2, 4.5, and 6.8 simulates what happens as the drug moves through your digestive system. This is especially critical for extended-release products and drugs that are pH-sensitive.
How does the FDA decide if a drug is BCS Class I?
A drug is classified as BCS Class I if it’s highly soluble in water and highly permeable across the intestinal wall. The FDA uses established criteria based on solubility thresholds and human absorption data. For these drugs, dissolution testing is simplified, and human bioequivalence studies are often waived, speeding up generic approval.
What happens if a generic drug fails dissolution testing?
The FDA issues a complete response letter, asking for more data or a reformulation. The company must revise the formulation, retest, and resubmit. This can delay approval by months or even years. In some cases, the product is never approved. The FDA prioritizes patient safety over speed.

I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.