When you pick up a generic pill from the pharmacy, you assume it works the same as the brand-name version. And for the most part, it does - same active ingredient, same effect, same price. But what you don’t see on the label might be causing real problems. Inactive ingredients - the fillers, dyes, and preservatives that hold the pill together - can interact in dangerous ways when you’re taking multiple generics at once. This isn’t theory. It’s happening right now, to real people.
What Are Inactive Ingredients, Really?
Inactive ingredients, or excipients, aren’t meant to treat anything. They’re there to make the drug stable, easy to swallow, or look the right color. Common ones include lactose, propylene glycol, tartrazine (a yellow dye), and bisulfites. Sounds harmless, right? But here’s the catch: every generic manufacturer picks their own mix. Two pills with the same active ingredient - say, metformin - can have completely different fillers. One might use lactose. Another might use corn starch. A third might use titanium dioxide for color.
The FDA doesn’t require generic drugs to match the inactive ingredients of the brand-name version. All they need to prove is that the active ingredient gets into your bloodstream within 80-125% of the original. That’s it. No checks on what’s holding the pill together. And with 90% of prescriptions in the U.S. filled with generics, the odds of mixing different excipients across multiple medications are extremely high.
Why This Matters More Than You Think
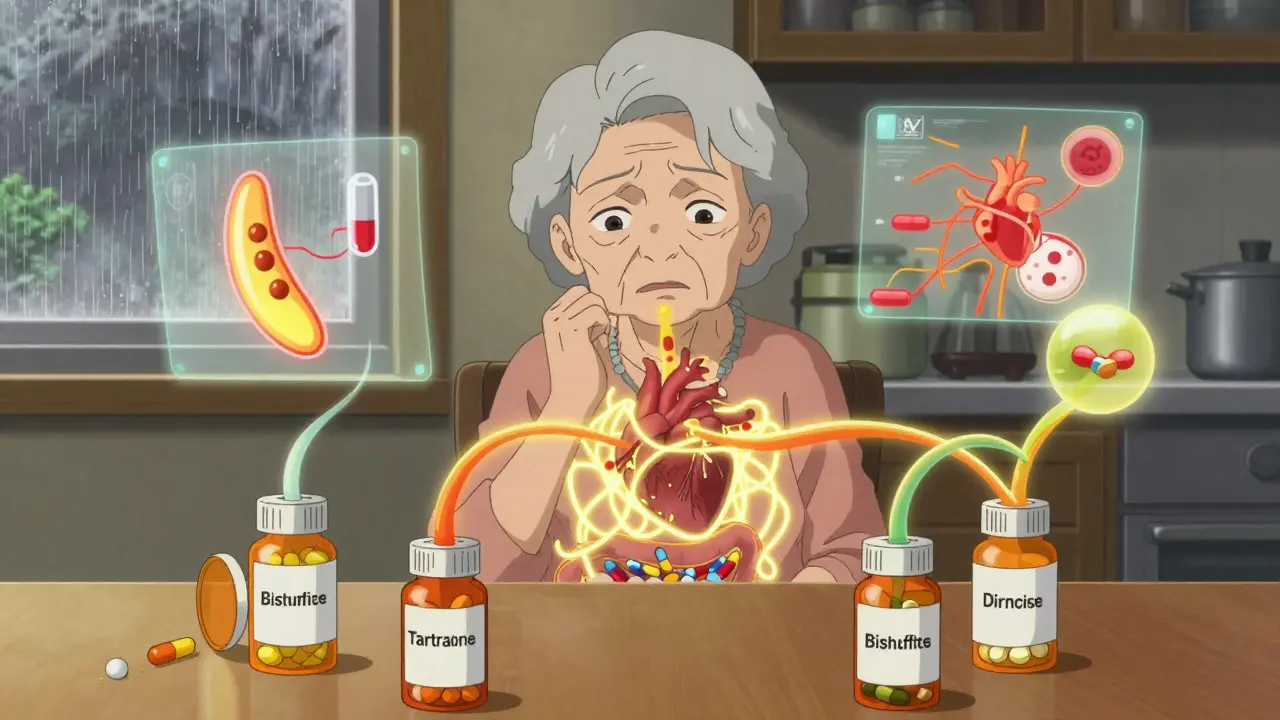
Imagine you’re on five different generic medications. Each one has a little bit of lactose - 50 mg here, 75 mg there. Individually, that’s fine. But add them up? You could be consuming 300-400 mg of lactose a day. For someone with lactose intolerance, that’s enough to trigger bloating, cramps, or diarrhea. And it’s not just lactose.
Propylene glycol is in nearly half of all liquid generics. In high doses, it can cause seizures or kidney issues - especially in kids or elderly patients. Tartrazine, a common yellow dye, triggers allergic reactions in about 4% of people. Bisulfites, used as preservatives, can cause asthma attacks in 5-10% of asthmatics. These aren’t rare side effects. They’re documented, predictable, and often missed because doctors and patients assume the problem is the active drug.
A 2020 study found that a person taking 10 prescriptions daily ingests an average of 2.8 grams of inactive ingredients every day. That’s over half a teaspoon of chemicals you didn’t ask for - and most of them aren’t listed in plain language on the bottle.
Real Cases, Real Consequences
There’s a Reddit thread from March 2023 with 147 comments from people who got sick after switching to generics. One user, u/MedSafetyWatcher, described months of unexplained stomach pain until they realized all three of their generic pills contained lactose. They’d been tolerating each one alone - but together, the dose crossed their personal threshold.
Another case: an elderly woman on digoxin - a heart medication with a narrow safety margin - started having irregular heartbeats after switching to a different generic version. Her blood levels were fine. But the new formulation used a different binder that slowed absorption. Her body wasn’t getting enough of the drug. She didn’t realize the change was in the filler, not the medicine.
The FDA’s Adverse Event Reporting System has thousands of reports labeled “unexplained GI distress,” “skin rash,” or “medication not working.” Many of these are likely excipient-related. Yet, most are dismissed as coincidence.
Brand vs. Generic: The Hidden Difference
Brand-name drugs often use the same excipients across batches. That consistency matters. Generics? Not so much. A 2021 FDA analysis found 27 different inactive ingredient combinations for generic levothyroxine - a thyroid hormone critical for metabolism. One version used corn starch. Another used mannitol. A third used magnesium stearate. All are approved. All are legal. But for someone with sensitivities, switching between them could mean daily discomfort or worse.
And the cost difference? Generics are 80-85% cheaper. That’s huge. But if you’re paying for side effects - doctor visits, ER trips, missed work - the real cost may be higher than you think.
Who’s at Risk?
Not everyone. But some groups are far more vulnerable:
- People with known allergies or intolerances (lactose, gluten, sulfites)
- Elderly patients on five or more medications
- Children, whose bodies process excipients differently
- Patients with autoimmune or chronic conditions (asthma, IBS, eczema)
- Those on drugs with narrow therapeutic windows - like digoxin, warfarin, or epilepsy meds
For example, a 2022 study showed a 15-20% drop in peak blood levels of certain antiepileptic drugs when switching from brand to generic - not because the active ingredient changed, but because the new formulation’s binder slowed absorption. That’s enough to trigger seizures.
What Can You Do?
You don’t have to stop taking generics. But you need to be smarter about them.
- Ask for the full ingredient list. Most pharmacies can pull it from the manufacturer’s database. Don’t settle for “it’s the same.”
- Track your excipients. Keep a list of every generic you take and note the fillers. Use apps like DailyMed or the FDA’s Inactive Ingredient Database. If you’re on three meds with lactose, ask your pharmacist if there’s a lactose-free version.
- Don’t switch generics without checking. Even if the name is the same, the filler might have changed. That’s why some people feel worse after a refill - not because the drug failed, but because the pill changed.
- Speak up if something feels off. Unexplained bloating? Rash? Headache? Tell your doctor or pharmacist. Say: “Could this be from the fillers?” Most won’t think of it - but you should.
A 2021 study in the American Journal of Health-System Pharmacy found that 78% of patients who identified problematic excipients and switched formulations saw their symptoms disappear. That’s not luck. That’s actionable insight.
The Bigger Picture
The generic drug market is growing fast - projected to hit $234 billion by 2027. More generics mean more combinations. More combinations mean more chances for hidden interactions.
Regulators are starting to wake up. The FDA launched the Inactive Ingredient Transparency Initiative in January 2024, requiring full digital labeling by December 2025. The European Medicines Agency already requires manufacturers to justify using excipients that affect more than 0.1% of the population. In the U.S., that’s still optional.
Some pharmacy chains now have “excipient awareness” protocols. But only 38% of independent pharmacies do. That means if you’re getting your meds from a small local pharmacy, you’re on your own.
And new tools are emerging. MedCheck AI, released in late 2023, scans your prescriptions and flags potential excipient conflicts with 89.7% accuracy. It’s not perfect - but it’s a start.
Final Thought: Your Meds Are More Complex Than You Think
Generic drugs saved billions in healthcare costs. That’s a win. But we’ve treated them like interchangeable parts - like swapping out a lightbulb. They’re not. Each pill is a custom blend of chemicals, chosen by a manufacturer with no obligation to match your body’s needs.
If you’re on multiple generics, especially if you have allergies, chronic illness, or are elderly - don’t assume safety just because it’s cheap. Ask questions. Track what’s in each pill. Advocate for yourself. Because sometimes, the thing making you sick isn’t the medicine.
It’s the filler.
Can inactive ingredients in generic drugs cause allergic reactions?
Yes. Common excipients like lactose, tartrazine, bisulfites, and propylene glycol can trigger allergic or intolerance reactions. Symptoms include hives, swelling, asthma attacks, or gastrointestinal distress. These reactions are often mistaken for side effects of the active drug, but they’re caused by the fillers.
Are generic drugs always safe if they have the same active ingredient?
Not always. While the active ingredient must be bioequivalent, the inactive ingredients can vary widely between brands and generics. These differences can affect how the drug is absorbed or trigger reactions in sensitive individuals - even if the active ingredient is identical.
How do I find out what’s in my generic medication?
Ask your pharmacist for the full inactive ingredient list. You can also look up your drug’s National Drug Code (NDC) on DailyMed.gov or the FDA’s Inactive Ingredient Database. The label on the bottle often omits details - so don’t rely on it alone.
Can switching between generic brands make my medication less effective?
Yes, especially for drugs with narrow therapeutic windows like digoxin, levothyroxine, or antiepileptics. Different binders or coatings can change how quickly the drug is absorbed, leading to under- or over-dosing. If your condition suddenly worsens after a refill, ask if the generic manufacturer changed.
Is there a way to avoid problematic excipients altogether?
You can reduce risk by sticking to one generic manufacturer for each drug, asking for formulations without common allergens (like lactose or dyes), or choosing brand-name versions if cost allows. Pharmacists can often source alternative generics with compatible excipients - but you need to ask.
Next Steps for Patients
If you’re on multiple generics, start today:
- Write down every medication you take - including over-the-counter ones.
- Call your pharmacy and ask for the inactive ingredients for each one.
- Look for repeats - especially lactose, propylene glycol, or artificial dyes.
- Ask your pharmacist: “Is there a version of this without [ingredient]?”
- Keep a note in your phone: “My meds contain X, Y, Z - avoid these.”
It takes 10 minutes. But it could prevent a hospital visit.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.