If you’ve ever stared at a pharmacy receipt and wondered how a small bottle of pills costs more than your monthly phone bill, you’re not alone. In the U.S., medication costs have become one of the most confusing and frustrating parts of healthcare. It’s not just about what’s on the label-it’s about coupons, generics, prior authorizations, and a system that often feels designed to keep you guessing. The good news? There are real ways to cut costs, and they don’t always involve waiting for government policy to change.
Why Your Prescription Costs So Much
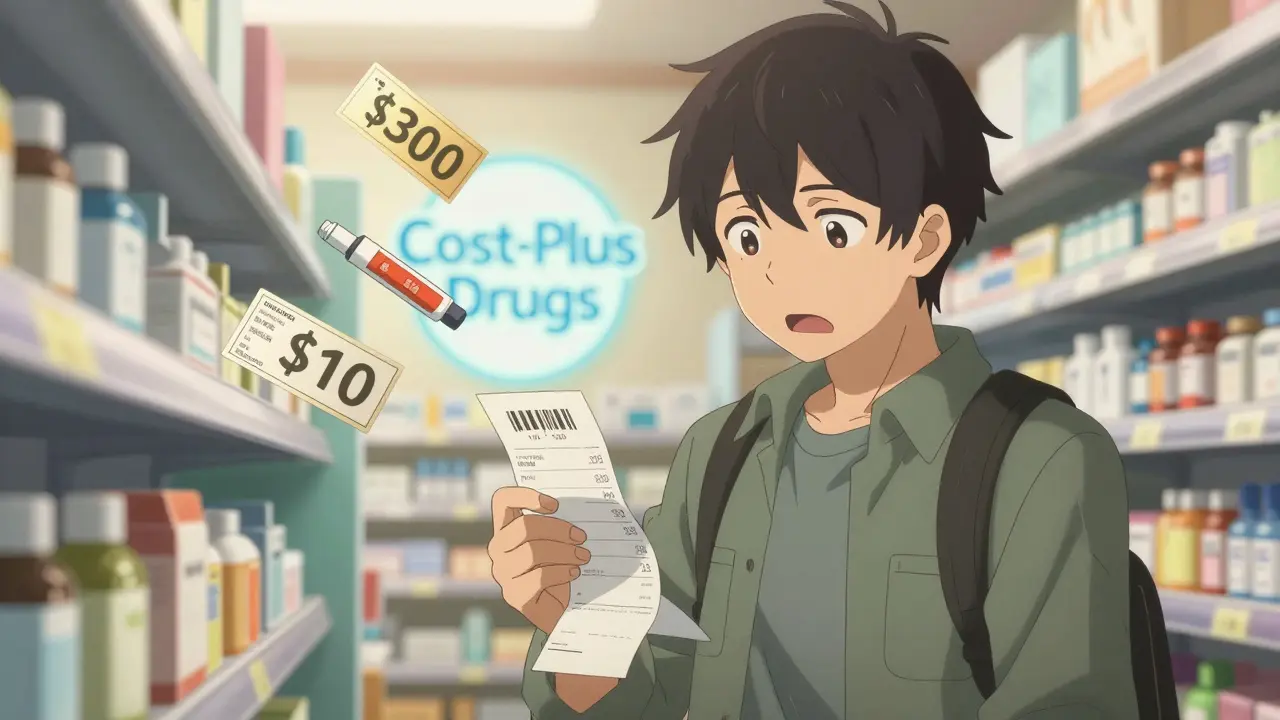
The price you see at the pharmacy isn’t the real price. It’s the list price, set by drugmakers and often inflated to make discounts look bigger. The actual price-what insurers and pharmacies pay-is called the net price. In 2025, Americans still pay two to three times more for the same drugs than people in Canada, Germany, or Australia. Why? Because the U.S. doesn’t regulate drug prices like most other developed countries. Instead, it relies on a tangled web of pharmacy benefit managers (PBMs), insurers, and rebates that rarely benefit the patient directly. Take a drug like insulin. A vial might list for $300, but your insurance might pay $70 after rebates. Yet you still pay $50 out of pocket because your plan has a high deductible. Meanwhile, Mark Cuban’s Cost-Plus Drugs sells the same insulin for $25 by cutting out middlemen and charging a flat service fee. No coupons. No mystery. Just cost-plus pricing.How Generic Drugs Can Save You Hundreds
Generic drugs are the most reliable way to cut medication costs. They’re chemically identical to brand-name drugs but cost 80% to 85% less. Yet many people stick with brand names out of habit-or because their doctor never mentioned the alternative. For example, the brand-name statin Lipitor costs around $200 a month without insurance. Atorvastatin, its generic version, runs about $10. That’s $2,280 saved per year. Same effectiveness. Same side effects. Same FDA approval. The only difference? The label. In 2025, over 90% of prescriptions filled in the U.S. were for generics. But not all generics are created equal. Some are made by the same companies that produce the brand-name versions. Others come from international manufacturers. The FDA requires all generics to meet the same standards, but if you notice a change in how you feel after switching, talk to your pharmacist. Sometimes, the filler ingredients differ slightly, and that can matter for sensitive patients.Prescription Coupons: Real Savings or Marketing Tricks?
You’ve seen them: “Save $50 on your next prescription!” These coupons, often handed out by drugmakers or found on websites like GoodRx, look like a gift. But here’s the catch: they only work if you’re paying cash or your insurance doesn’t cover the drug. If you use insurance, the coupon might not apply at all-or worse, it could count toward your deductible without reducing your overall cost. Worse still, some coupons are designed to lock you into expensive brand-name drugs. A drugmaker might offer a $100 coupon for a $400 medication, making it seem like a steal. But if a $15 generic exists, you’re still paying $285 more than you need to. The smart move? Always compare the coupon price to the cash price at different pharmacies, then check if your insurance can do better. Use GoodRx or SingleCare to see real-time prices. Often, the cash price without a coupon is lower than the coupon price with insurance.
Prior Authorization: The Hidden Gatekeeper
Prior authorization is when your insurance demands proof that you’ve tried cheaper options before approving a pricey drug. It sounds reasonable-until you’re waiting two weeks for approval while your condition worsens. Let’s say your doctor prescribes a new GLP-1 weight-loss drug like Ozempic. Your insurer says, “Try metformin first.” But you already tried metformin. It gave you nausea and didn’t work. Now you need a letter from your doctor, lab results, and a form signed by your provider. All before you can fill the prescription. This system is broken. PBMs and insurers use prior authorization to control costs-but the burden falls on patients and providers. In 2025, the average prior authorization request took 4.7 days to process. For urgent conditions, that’s too long. Some states now require insurers to approve or deny requests within 72 hours for urgent cases. But enforcement is patchy. Tip: Ask your doctor to submit the prior authorization request the same day they write the prescription. Many clinics now have staff dedicated to this. If your claim gets denied, appeal immediately. Most denials are overturned on appeal.Medicare’s Big Changes in 2025-2026
If you’re on Medicare, 2025 was a turning point. The Inflation Reduction Act introduced a $2,000 annual out-of-pocket cap on Part D drugs. That means no more “donut hole” surprises. You’ll pay nothing after hitting that cap. Also in 2026, Medicare will start negotiating prices for 10 high-cost drugs, including Eliquis, Xarelto, and Januvia. The negotiated prices will be about 22% lower than 2023 levels. That translates to an average $400 annual savings per Medicare beneficiary. These changes are just the start. By 2029, Medicare will negotiate up to 60 drugs per year. And for the first time, the government is pushing to extend these lower prices to Medicaid and commercial insurers. That could save the entire system over $1 trillion over ten years.
What You Can Do Right Now
You don’t have to wait for policy changes to save money. Here’s what works today:- Ask for the generic. Always. Even if your doctor doesn’t mention it.
- Compare prices. Use GoodRx, SingleCare, or your pharmacy’s app. Prices vary wildly-even between two CVS locations.
- Use mail-order pharmacies. Many insurers offer 90-day supplies at lower copays. You’ll pay less per pill and avoid frequent trips.
- Check for patient assistance programs. Drugmakers like Pfizer, AbbVie, and Roche offer free or discounted drugs to low-income patients. Go to NeedyMeds.org to find programs.
- Don’t skip doses to save money. That’s dangerous. Instead, talk to your doctor about switching to a cheaper alternative.
When Coupons Backfire
A lot of people think coupons are free money. They’re not. Some coupons are structured so that your insurance doesn’t count the payment toward your deductible. That means you’re still paying full price after the coupon expires. Worse, some coupons only apply to brand-name drugs, even when a generic exists. That’s not saving money-it’s subsidizing corporate profits. Always ask: “Is there a cheaper version?” and “Will this coupon reduce my overall spending, or just make the sticker price look better?”The Future of Drug Pricing
The U.S. is slowly moving away from the old model of sky-high list prices and secret rebates. The GENEROUS Model for Medicaid is testing international price benchmarks. States like Minnesota are using Medicare negotiation prices as upper limits for what they’ll pay. And companies like Cost-Plus Drugs are proving that transparent pricing works. But change moves slowly. Until then, your best tools are knowledge and persistence. Know your options. Ask questions. Push back when something doesn’t make sense. You’re not powerless. You just need to know how the system really works.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent, meaning they work the same way in your body. The only differences are in inactive ingredients like fillers or dyes-which rarely affect how the drug works. Millions of people take generics safely every day.
Can I use a coupon with my insurance?
Sometimes, but not always. Most manufacturer coupons are designed for cash-paying patients. If you use insurance, the coupon may not apply-or it might count toward your deductible without lowering your overall cost. Always check with your pharmacist before using a coupon. In many cases, the cash price without a coupon is cheaper than the coupon price with insurance.
Why does my pharmacy charge different prices for the same drug?
Pharmacies negotiate different prices with pharmacy benefit managers (PBMs), and each plan has its own pricing structure. A drug might cost $15 at Walmart, $35 at CVS, and $20 at your local independent pharmacy-even with the same insurance. Always compare prices using tools like GoodRx before filling your prescription.
What should I do if my prior authorization is denied?
Don’t accept the denial. Ask your doctor to file an appeal. Most denials are overturned on appeal, especially if you provide documentation showing you’ve tried cheaper alternatives or that the drug is medically necessary. Keep copies of all paperwork. You have the right to a written explanation and a fast review if your condition is urgent.
Is it safe to buy medications from online pharmacies?
Only buy from pharmacies verified by the National Association of Boards of Pharmacy (NABP). Look for the VIPPS seal (Verified Internet Pharmacy Practice Sites). Many online pharmacies sell counterfeit or expired drugs. Even if the price looks too good to be true, it probably is. Stick to licensed U.S. pharmacies or those with clear regulatory oversight.
How do I know if I qualify for patient assistance programs?
Most programs are based on income and insurance status. If you’re uninsured, underinsured, or have a low household income, you likely qualify. Programs from drugmakers like Pfizer, Merck, and Novo Nordisk offer free or deeply discounted medications. Visit NeedyMeds.org or call the manufacturer’s patient support line directly. Many require a simple application and proof of income.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.