Osteonecrosis of the Jaw Risk Assessment Tool
Your Personal ONJ Risk Assessment
This tool helps you understand your risk of developing medication-related osteonecrosis of the jaw based on your medications and symptoms. It's not a substitute for professional medical advice.
Your Risk Assessment Results
When you’re taking medication for osteoporosis or cancer that’s spread to your bones, you’re likely focused on how it’s helping you live longer or stay stronger. But there’s a silent risk hiding in your mouth-one that can start with a simple toothache and turn into something life-altering. It’s called osteonecrosis of the jaw, or MRONJ for short. And while it’s rare, the consequences are serious. If you’re on certain drugs, your jawbone can start dying without warning. The good news? You can spot the early signs before it gets bad-if you know what to look for.
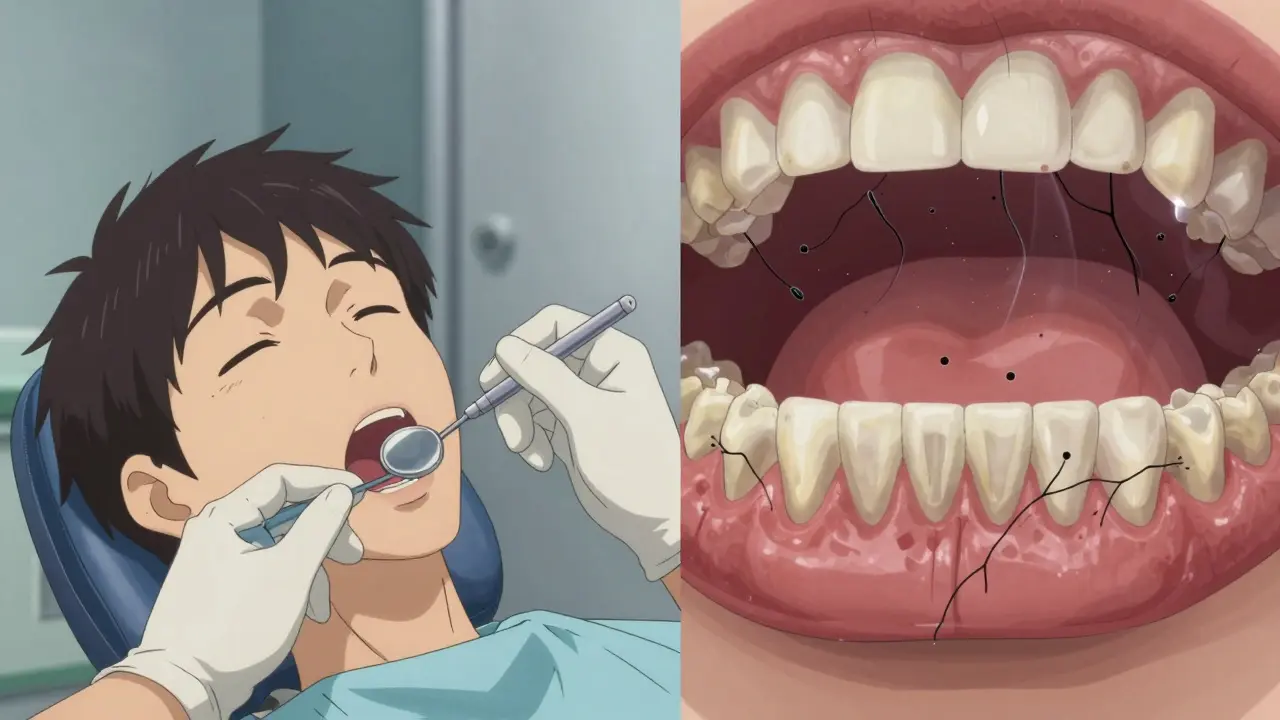
What Exactly Is Osteonecrosis of the Jaw?
Osteonecrosis of the jaw isn’t just a dental infection. It’s when the bone in your upper or lower jaw stops healing and dies, leaving exposed bone in your mouth for more than eight weeks. It doesn’t heal on its own. And it’s almost always tied to medications that slow down bone turnover. These include bisphosphonates like alendronate (Fosamax), ibandronate (Boniva), and zoledronate (Reclast), as well as denosumab (Prolia) and romosozumab. These drugs are lifesavers for people with osteoporosis or cancer that’s spread to the bones. But they also make your jawbone more fragile by stopping the natural process of bone repair.
Think of your jawbone like a tree. Normally, roots grow and repair themselves over time. But these medications act like a freeze button on that repair system. So when you have a tooth pulled, a denture rubs raw, or even a small gum infection develops, your body can’t fix the damage. The bone starts to die. And because your mouth is full of bacteria, infection sets in. That’s when things get dangerous.
The Top 6 Warning Signs You Need to Watch For
Most people don’t realize they’re at risk until they’re already in pain. But the early signs are clear-if you know what to look for. Here are the six most common warning signs of medication-related osteonecrosis of the jaw:
- Pain or swelling in your mouth-not just a toothache, but a deep, persistent ache that doesn’t go away with painkillers. In 87% of cases, this is the first symptom reported.
- Slow or failed healing after a tooth extraction-if your gums aren’t closing up two weeks after a pull, or if you see bone sticking out, that’s a red flag. People on these meds are 3.2 times more likely to develop ONJ after an extraction than those who aren’t.
- Loose teeth for no clear reason-if your teeth suddenly feel wobbly and you haven’t had gum disease before, it could be the bone beneath them weakening.
- Visible bone in your mouth-this is the defining feature. If you can see white or gray bone through your gums, especially after a dental procedure, it’s not normal. It’s ONJ.
- Pus or foul-smelling discharge from your gums-a sign of infection that won’t clear up with antibiotics alone. This happens in 58% of cases.
- Numbness or heaviness in your jaw-like your jaw is full of lead. It’s not just soreness. It’s a deep, strange sensation that doesn’t match any typical dental issue. Seen in 42% of diagnosed cases.
These symptoms don’t always show up right away. Sometimes they creep in months after you started your medication. That’s why it’s so easy to miss. Many patients think it’s just a bad infection and keep going to the dentist for antibiotics. But if the bone is dead, antibiotics won’t fix it. Only early detection can stop it from getting worse.
Which Medications Carry the Highest Risk?
Not all medications are created equal when it comes to jaw damage. The risk depends on the drug, the dose, and how it’s given.
People taking intravenous bisphosphonates for cancer-like zoledronate given monthly in a hospital-are at the highest risk. Studies show 1% to 10% of these patients develop ONJ. That’s 100 to 1,000 times higher than people taking oral pills for osteoporosis.
For those on oral bisphosphonates like Fosamax or Boniva, the risk is tiny-between 0.001% and 0.01%. That’s about 1 in 10,000 to 1 in 100,000 people per year. Still, because so many people take these drugs, even that small percentage adds up. And the risk goes up the longer you’re on them. After three to four years, the chance of ONJ doubles.
Denosumab (Prolia), a newer drug used for osteoporosis, carries a similar risk to oral bisphosphonates. But here’s the catch: if you stop taking it, your bone turnover can rebound quickly. That’s why dental work after stopping denosumab needs extra caution.
And here’s something most patients don’t know: you don’t need a major procedure to trigger ONJ. A simple cleaning, a loose crown, or even a denture that rubs too hard can be enough-especially if you’ve been on the meds for years.
What Should You Do Before Starting These Medications?
The best way to avoid ONJ is to prevent it before you even start the drug. If your doctor is about to prescribe an intravenous bisphosphonate or denosumab for cancer, or even a strong oral bisphosphonate for osteoporosis, you need a full dental checkup 4 to 6 weeks before your first dose.
That’s not a suggestion-it’s a medical standard. The American Dental Association says it clearly: get every cavity filled, every infected tooth pulled, every denture adjusted before you start. Why? Because once you’re on the medication, your body can’t heal properly. Any dental work done after that carries a much higher risk of complications.
If you’re already on the medication, don’t panic. You don’t need to stop your treatment. But you do need to tell every dentist you see-every single time-that you’re taking these drugs. Many dentists don’t ask. And if they don’t know, they won’t take the extra precautions.
Also, avoid invasive procedures if you can. Routine cleanings and fillings are safe. But extractions, implants, and bone surgeries should be avoided unless absolutely necessary. If you need one, your doctor might recommend a short break from the medication-usually 2 to 3 months for intravenous drugs. That’s not always possible for cancer patients, but it’s something to discuss.
How to Protect Yourself While on These Drugs
If you’re already taking one of these medications, here’s what you can do right now to lower your risk:
- Use chlorhexidine mouthwash-twice a day. A 2021 study showed it cuts ONJ risk by 37% in high-risk patients.
- Keep your gums healthy-brush gently, floss daily, and avoid tobacco. Poor oral hygiene increases your risk dramatically.
- Get dental checkups every 6 months-even if nothing hurts. Early detection saves your jaw.
- Don’t ignore minor pain-if your tooth or gum hurts for more than a week, see your dentist. Don’t wait for it to get worse.
- Ask for a dental clearance letter-if you’re switching doctors or starting a new medication, ask your dentist to write a note confirming your mouth is healthy.
And here’s something most people don’t realize: your dentist and your oncologist or rheumatologist need to talk to each other. If they don’t, you’re the one who pays the price. Don’t be afraid to say, “Can you two coordinate my care?”
What Happens If It’s Already Advanced?
If ONJ has already progressed, treatment is harder. In early stages (Stage 1), doctors may use mouth rinses, antibiotics, and careful cleaning. In later stages (Stage 2 or 3), you might need surgery to remove dead bone. Some patients end up losing part of their jaw. Others can’t eat normally for months.
But there’s hope. New research from UCSF shows that teriparatide (Forteo), a bone-building drug, can help heal early-stage ONJ in 78% of cases-far better than standard care. It’s not yet standard treatment, but it’s being tested widely. And the NIH is developing a tool called the Osteonecrosis Prediction Algorithm (OPA), which could soon tell you your personal risk based on your genes, medication history, and dental health. That’s coming by 2025.
For now, the key is awareness. The more people know, the fewer will suffer.
Why So Many People Miss the Signs
One of the biggest problems? Misdiagnosis. On patient forums, 89% of people with ONJ say their dentist first thought it was just a regular infection. They got antibiotics. The pain went away for a bit. Then it came back. Months later, they finally saw an oral surgeon-and it was too late.
And here’s the scary part: 73% of patients on Reddit said their dentist never asked if they were taking osteoporosis or cancer meds. That’s not negligence-it’s ignorance. But it’s changing. In 2015, only 42% of U.S. dental schools taught about ONJ. Now, 87% do. Still, private practices lag behind. If you’re seeing a dentist outside a hospital or university clinic, you might be the one who has to educate them.
Don’t wait for them to ask. Say it first: “I’m on Fosamax/Prolia. I need you to check for bone exposure.”
Can osteonecrosis of the jaw happen without a dental procedure?
Yes. While most cases start after tooth extraction or denture trauma, about 15% of ONJ cases occur spontaneously-without any obvious trigger. This is more common in patients on long-term intravenous bisphosphonates for cancer. Even minor gum irritation or a small ulcer can be enough to start the process if bone turnover is severely suppressed.
Is ONJ reversible?
In early stages, yes-with the right care. Stopping the medication (if possible), using chlorhexidine rinses, and sometimes adding teriparatide can help the bone heal. But once large areas of bone are dead, they can’t come back to life. Surgery may be needed to remove the damaged tissue. Early detection is the only way to avoid major procedures.
Should I stop my osteoporosis or cancer medication to avoid ONJ?
No-not without talking to your doctor. The risk of ONJ is very low for most people on oral bisphosphonates, and the benefits of preventing broken bones or cancer spread far outweigh the risk. Stopping these drugs can lead to fractures, spinal collapse, or faster cancer progression. Focus on prevention: get a dental checkup before starting, and maintain great oral hygiene.
Can I still get dental cleanings if I’m on these medications?
Absolutely. Routine cleanings, fillings, and crowns are safe and encouraged. In fact, keeping your mouth healthy reduces your risk of ONJ. The danger comes from invasive procedures like extractions or implants. Always tell your dentist you’re on bisphosphonates or denosumab before any treatment.
How long after starting the medication does ONJ usually appear?
For cancer patients on IV bisphosphonates, ONJ often develops within 6 to 12 months after starting treatment-especially after a dental procedure. For osteoporosis patients on oral meds, it usually takes 3 to 5 years. But it can happen anytime, even after 10 years. That’s why ongoing dental care is critical.
Final Takeaway: Knowledge Is Your Shield
You’re not alone if you’re worried. Thousands of people take these medications every year without ever developing ONJ. But for those who do, the delay in diagnosis is almost always the same: they didn’t know what to look for, and no one told them to ask.
If you’re on one of these drugs, your jaw is a silent warning system. Pay attention to it. Talk to your dentist. Tell your doctor. Don’t wait for pain to become unbearable. The goal isn’t to scare you-it’s to give you control. With the right awareness, you can protect your jaw, your health, and your quality of life-while still getting the full benefit of your medication.


I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.