SVT Symptom Checker
Check Your Symptoms
Answer the following questions about your symptoms to get personalized guidance on whether you should seek medical attention.
Your Symptom Analysis
Quick Summary
- SVT is a fast heart rhythm that starts above the ventricles and often feels like a sudden racing heartbeat.
- Typical signs include palpitations, shortness of breath, dizziness or chest pressure.
- Diagnosis relies on an electrocardiogram (ECG) and sometimes an electrophysiology study.
- First‑line treatment includes vagal maneuvers and medications such as beta‑blockers or adenosine.
- Catheter ablation offers a long‑term cure for many patients who have frequent episodes.
What is Supraventricular Tachycardia?
When you hear the term supraventricular tachycardia is a rapid heart rhythm that originates above the ventricles, typically in the atria. The atria are the two upper chambers of the heart, and they normally send a measured electrical signal to the lower chambers, the ventricles. In SVT, an extra circuit or a premature beat triggers a cascade that makes the heart beat excessively fast-often 150 to 250 beats per minute.
Because the problem starts “above” the ventricles, the condition is called “supraventricular.” It’s a type of arrhythmia, which is any irregularity in the heart’s rhythm. While most SVT episodes are not life‑threatening, they can be scary and may cause symptoms that affect daily life.
Common Symptoms & When to Seek Help
People with SVT usually notice a sudden onset of a fast heartbeat. Typical symptoms include:
- Palpitations-feeling like the heart is pounding or fluttering.
- Shortness of breath, especially during an episode.
- Dizziness or light‑headedness; in rare cases, fainting.
- Chest discomfort or pressure (often mistaken for heart attack).
- Fatigue after an episode resolves.
If any of these symptoms appear out of the blue, especially in a younger adult without known heart disease, it’s wise to visit a clinician. Persistent or worsening chest pain, trouble breathing at rest, or fainting require immediate medical attention.
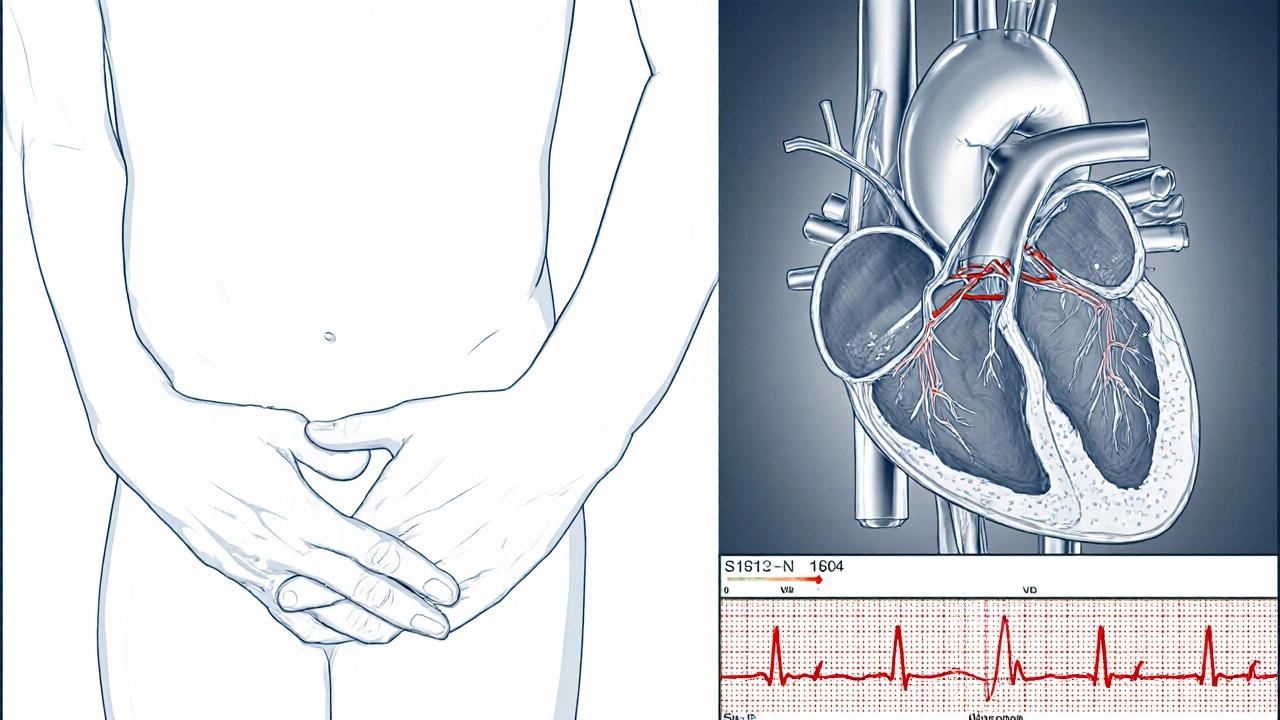
How Doctors Diagnose SVT
The gold‑standard test is an electrocardiogram (ECG). During an episode, the ECG shows a characteristic pattern: narrow QRS complexes with a rapid rate. If an episode isn’t happening in the office, doctors may use a Holter monitor (24‑48hour ECG) or an event recorder that the patient activates when symptoms start.
When the diagnosis remains unclear, an electrophysiology study (EPS) may be performed. In an EPS, thin catheters are threaded through the veins to the heart, and tiny electrical signals map the exact pathway that’s causing the rapid rhythm. This invasive test not only confirms SVT but also helps plan a possible ablation.
Treatment Options Overview
Treatment follows a step‑wise approach: first, simple maneuvers that can break the circuit; second, medication to control the rate; and finally, invasive procedures for a long‑term solution. The choice depends on how often episodes occur, how severe the symptoms are, and the patient’s overall health.
Medication Options
Several drug classes are routinely used:
- Beta‑blockers (e.g., metoprolol, atenolol) slow the heart by blocking adrenaline’s effect.
- Calcium channel blockers (e.g., diltiazem, verapamil) reduce the speed of electrical conduction in the atria.
- Adenosine is given intravenously in a rapid push; it briefly pauses the heart’s conduction system and can often terminate an SVT episode on the spot.
These medicines have different side‑effect profiles. Beta‑blockers may cause fatigue or low blood pressure; calcium channel blockers can lead to constipation or swelling; adenosine may cause a brief sensation of flushing or chest tightness-but the effect wears off in seconds.
Non‑Medication Strategies
Before reaching for pills, many patients successfully stop an episode with vagal maneuvers. Simple actions that stimulate the vagus nerve include:
- Valsalva maneuver - exhale against a closed airway for 15 seconds.
- Cold water face immersion - dunk your face in ice‑cold water for 10‑15 seconds.
- Carotid sinus massage - gentle pressure on the neck (only by a trained professional).
If episodes recur despite maneuvers and medication, a catheter ablation may be recommended. During ablation, a tiny tip delivers radio‑frequency energy to destroy the tiny tissue responsible for the errant circuit. Success rates for typical AV‑nodal re‑entrant tachycardia (a common SVT type) exceed 95%, and most patients return to normal activity within a few days.
In very rare cases where the heart’s conduction system is damaged, a pacemaker may be implanted to keep the heart beating at a safe minimum rate.
Comparing Medication & Ablation
| Option | Typical Use | Effectiveness % | Key Side Effects | Invasiveness |
|---|---|---|---|---|
| Vagal Maneuvers | First‑line, acute termination | 30‑50 (when successful) | None (rare light‑headedness) | Non‑invasive |
| Beta‑blockers | Pre‑vention, chronic control | 70‑80 | Fatigue, low BP | Oral medication |
| Calcium Channel Blockers | Pre‑vention, chronic control | 65‑75 | Constipation, edema | Oral medication |
| Adenosine (IV) | Acute termination in ER | 90‑95 | Flushing, brief pause | IV administration |
| Catheter Ablation | Long‑term cure for recurrent SVT | 95‑98 | Vascular injury, rare heart block | Minimally invasive procedure |
Lifestyle & Trigger Management
Even after successful treatment, many patients find that certain habits can provoke an SVT episode. Common triggers include:
- Excess caffeine or energy drinks.
- Alcohol bingeing, especially on an empty stomach.
- Heavy cigarettes or vaping nicotine.
- Emotional stress or anxiety spikes.
- Dehydration and electrolyte imbalance.
Keeping a simple diary-recording when an episode occurs, what you ate, your stress level, and any meds taken-helps you and your cardiologist spot patterns. Regular aerobic exercise, adequate sleep, and a balanced diet support overall cardiac health and can reduce the frequency of SVT episodes.
Frequently Asked Questions
Can SVT be fatal?
Most SVT forms are not life‑threatening, but extremely rapid rates can reduce cardiac output and cause fainting. Prompt treatment and follow‑up keep the risk low.
Is SVT hereditary?
A small number of SVT cases run in families, suggesting a genetic predisposition to the electrical pathways involved. However, most cases arise without a clear family link.
How long does a catheter ablation recovery take?
Most patients are discharged the same day or after an overnight stay. Light activity can resume within a day, and normal exercise is usually cleared after one to two weeks.
Are there any foods that help prevent SVT?
There’s no magic food, but a diet low in caffeine, alcohol, and high‑sugar snacks, paired with plenty of potassium‑rich fruits (bananas, avocados) and magnesium (nuts, leafy greens), supports stable heart rhythms.
Can pregnancy worsen SVT?
Hormonal changes and increased blood volume can raise heart rate, sometimes triggering more SVT episodes. Management is similar, but medication choices are limited to those proven safe in pregnancy.
Bottom Line
Understanding what triggers your SVT, how it’s diagnosed, and the range of treatment options empowers you to work with your doctor toward a plan that fits your lifestyle. Whether a simple Valsalva, a daily beta‑blocker, or a one‑time ablation, each step moves you closer to a steadier heartbeat and fewer scary episodes.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.