When a child or adult breaks out in a rash while taking an antibiotic, panic often kicks in. Parents rush to stop the medicine. Adults cancel their next dose. But here’s the hard truth: most antibiotic rashes aren’t allergic reactions. And stopping the drug unnecessarily can do more harm than good.
Not All Rashes Are Allergies
Let’s clear this up right away. If you or your child gets a rash while on amoxicillin or another penicillin-based antibiotic, it’s likely not an allergy. Studies show that 90% of kids labeled as allergic to amoxicillin because of a rash turn out to be fine when tested properly. That’s not a small number-it’s the majority.
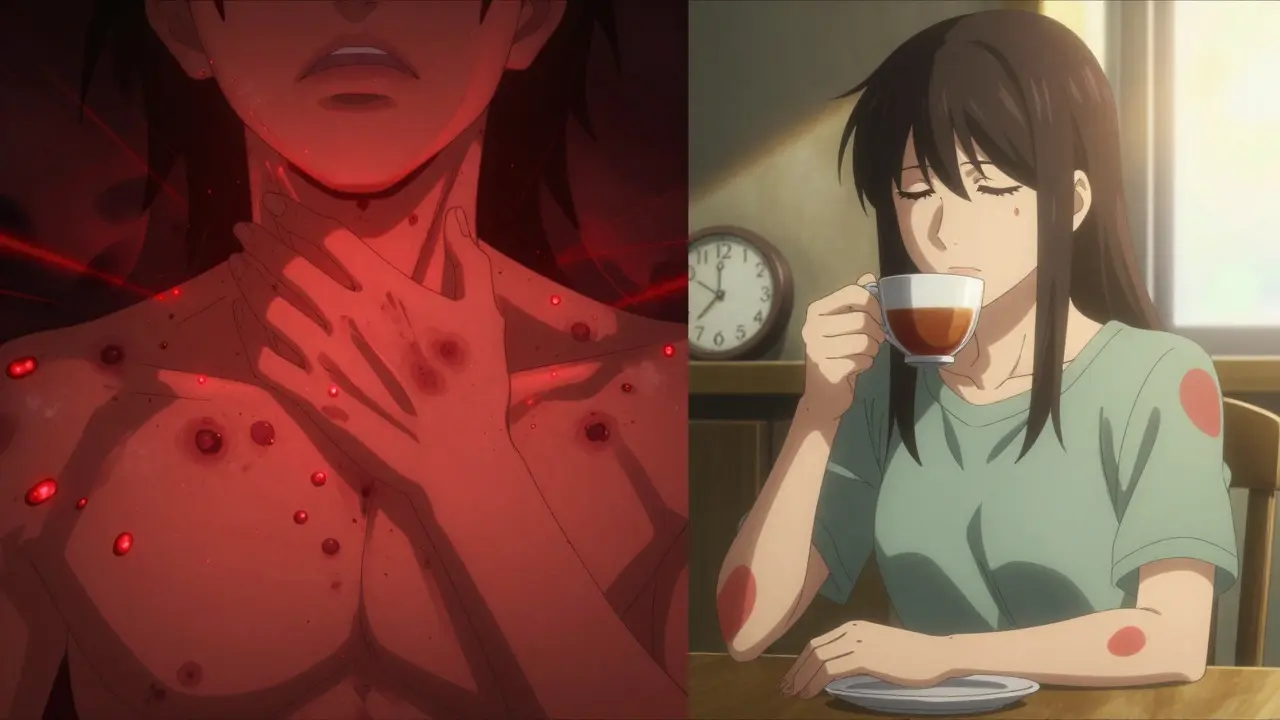
The rash usually shows up between days 5 and 10 of treatment. It’s flat, red, patchy, and not very itchy. It often starts on the trunk and spreads to the arms or legs. It doesn’t move around. It doesn’t swell. It just… sits there. This is called a maculopapular rash. It’s not dangerous. It’s not an allergy. It’s the body’s weird response to the combination of the antibiotic and a recent virus-like a cold or the flu.
Meanwhile, true allergic reactions look completely different. These show up within an hour of taking the drug. The skin erupts in raised, red, swollen welts-hives-that itch intensely. They come and go, changing shape and location. Sometimes the lips or tongue swell. Breathing gets hard. This is a medical emergency. If you see this, stop the antibiotic immediately and call for help.
What to Do When the Rash Appears
Here’s the simple checklist you need to follow the moment you notice a rash:
- Check the timing. Did it show up before day 5? If yes, it’s more likely an allergy. If it’s day 7 or later, it’s probably harmless.
- Look at the rash. Are the bumps flat and spread out? Keep taking the antibiotic. Are they raised, bumpy, and super itchy? Call your doctor.
- Watch for other symptoms. Fever? Swollen lymph nodes? Blisters in the mouth? Eyes or throat swelling? These are red flags. Stop the drug and go to urgent care.
- Don’t assume. Just because you had a rash once doesn’t mean you’re allergic forever. Most people outgrow this.
One study of over 2,400 children found that 78% of non-allergic rashes appeared between days 5 and 10. That’s not random-it’s predictable. If you’re on day 3 and get a rash, be cautious. On day 8? Probably fine.
When to Stop the Antibiotic
You should stop the antibiotic only if:
- The rash is raised, itchy, and moving around (hives)
- You have trouble breathing, wheezing, or swelling in the throat
- You develop blisters, peeling skin, or sores in your mouth, eyes, or genitals
- You have a fever over 38.5°C (101.3°F) with swollen glands
These signs point to serious conditions like Stevens-Johnson Syndrome (SJS), toxic epidermal necrolysis (TEN), or DRESS syndrome. These are rare-only 1 to 6 cases per million prescriptions-but they can be deadly. If any of these happen, stop the drug, call 999, and go to the ER.
For everything else? Keep taking the antibiotic. The infection won’t treat itself. Stopping early increases the chance of the infection coming back worse-and often requires stronger, more expensive antibiotics like clindamycin or vancomycin. These carry higher risks of severe diarrhea, including Clostridioides difficile infection, which can land you in the hospital.
What to Do for Comfort
If the rash is non-allergic and not bothering you, you don’t need to treat it. It will fade on its own in 5 to 7 days. But if it’s itchy, here’s what actually works:
- Take an H1 antihistamine like cetirizine (Zyrtec) or loratadine (Claritin). One dose a day is enough.
- Use H2 antihistamine like famotidine (Pepcid) if the itching is stubborn. This combo works better than either alone.
- Apply 1% hydrocortisone cream to itchy spots. Don’t overuse it-just a thin layer twice a day.
- A cool bath with oatmeal or baking soda can help soothe the skin.
Don’t use oral steroids unless a doctor tells you to. Studies show they don’t speed up healing and can even make things worse in some cases.
Why Mislabeling Rashes Is Dangerous
When people get labeled as “allergic to penicillin” after a harmless rash, it changes their medical care forever. Doctors avoid the safest, cheapest, and most effective antibiotics. Instead, they reach for alternatives like azithromycin, clindamycin, or fluoroquinolones.
These alternatives are less targeted. They wipe out good bacteria. They cause more diarrhea. They increase the risk of C. diff infection by 30%. They cost 69% more. And in life-threatening infections like sepsis, patients with mislabeled allergies have a 30% higher risk of death.
The CDC estimates that in the U.S. alone, this one mistake costs the healthcare system $1.2 billion every year. It’s not just about money-it’s about survival.
What Your Doctor Should Do Next
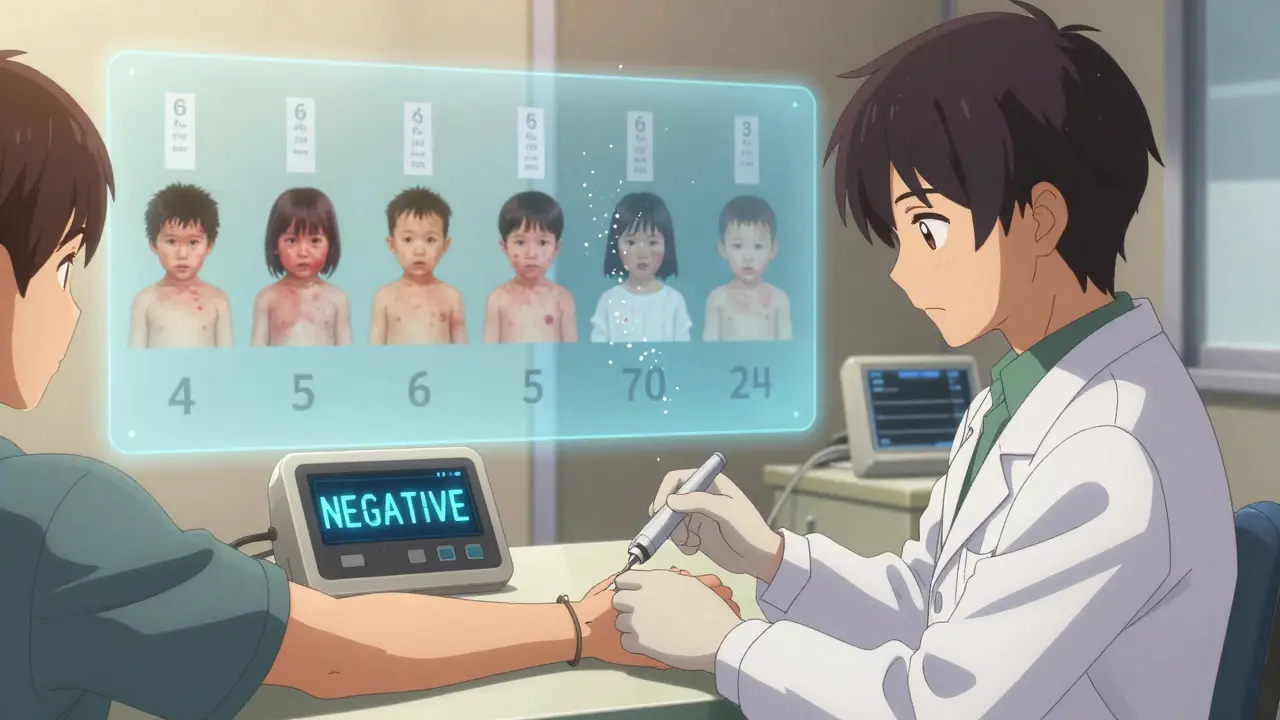
If you’ve been told you’re allergic to penicillin because of a childhood rash, ask about allergy testing. It’s simple. A skin test takes 15 minutes. A blood test takes a day. Both are accurate. And if you test negative? You can safely take penicillin again.
New tools are making this easier. The FDA approved a rapid penicillin allergy test called PENtest in 2023. It gives results in 15 minutes instead of 3 hours. Hospitals across the UK and US are starting to use it. You don’t need to live in a big city to get it-many GP clinics now offer it.
Also, ask your doctor to update your medical record. Don’t let them write “penicillin allergy” unless it’s confirmed. Write instead: “Rash on day 7 of amoxicillin-no anaphylaxis, no hives.” This small change saves lives.
Real Stories, Real Consequences
A mom on Reddit stopped amoxicillin when her 4-year-old got a rash on day 3. Two weeks later, the ear infection returned worse. She had to switch to clindamycin. The child got severe diarrhea that lasted two weeks. She later learned the rash was non-allergic.
A nurse shared a different story: her niece got the same rash on day 8. The doctor said to keep going. The rash faded in five days. The infection cleared. No complications.
One survey found that 79% of parents thought any rash meant an allergy. Only 17% called their doctor first. The rest guessed. And guessing wrong can be costly.
Bottom Line
Most antibiotic rashes aren’t dangerous. Most are harmless. Most don’t need stopping. But some are life-threatening. The difference comes down to details: timing, appearance, and symptoms.
Don’t stop your antibiotic just because of a rash. Call your doctor. Describe it. Send a photo if you can. Let them guide you. If they say keep going-do it. The infection matters more than the rash.
And if you’ve been told you’re allergic to penicillin because of a childhood rash? Get tested. You might be surprised.
Is an antibiotic rash always an allergy?
No. In fact, most are not. Around 90% of rashes from amoxicillin in children are non-allergic. These rashes appear days after starting the drug, are flat and not itchy, and don’t come with other symptoms. True allergic reactions are rare and happen within an hour, with raised, itchy hives and possible breathing trouble.
Should I stop taking the antibiotic if I get a rash?
Only if the rash is raised, itchy, spreading quickly, or if you have swelling, trouble breathing, fever over 38.5°C, or blisters in your mouth or eyes. If the rash is flat, appears after day 5, and doesn’t bother you, keep taking the antibiotic. Stopping it unnecessarily increases the risk of treatment failure and more dangerous side effects.
Can I take penicillin again if I had a rash once?
Yes, most people can. If your rash happened years ago and you never had another reaction, you’re likely not allergic. A simple skin or blood test can confirm this. Many adults who think they’re allergic to penicillin test negative. Getting tested removes unnecessary restrictions and opens up safer treatment options.
What’s the difference between hives and a non-allergic rash?
Hives are raised, red, itchy bumps that change shape and location within hours. They often appear within 1 hour of taking the drug. Non-allergic rashes are flat, red patches that don’t move, don’t itch much, and appear 5-10 days after starting the antibiotic. Hives = stop the drug. Flat rash = keep going.
Can antihistamines help with an antibiotic rash?
For non-allergic rashes, antihistamines only help with itching-they don’t make the rash go away faster. Cetirizine (Zyrtec) or loratadine (Claritin) once daily, plus famotidine (Pepcid) if needed, can ease discomfort. Topical hydrocortisone cream can also help. But don’t expect the rash to vanish sooner. It will fade on its own.
Why is it bad to stop an antibiotic because of a rash?
Stopping an antibiotic early increases the chance the infection returns, often worse than before. You may need a stronger, broader-spectrum antibiotic like clindamycin or vancomycin, which cause more side effects-especially severe diarrhea from C. diff. Studies show patients who stop antibiotics due to rash have a 63% higher risk of this infection. It’s safer to finish the course unless it’s a true allergic reaction.
Is there a test to confirm if I’m allergic to penicillin?
Yes. A skin test with a small amount of penicillin is the gold standard. It takes 15 minutes and is over 95% accurate. A blood test is also available. These tests are now widely available in GP clinics and hospitals. If you were told you’re allergic because of a childhood rash, getting tested can change your medical care for the better.
Can antibiotic rashes happen in adults too?
Yes. While more common in children, especially those with viral infections like Epstein-Barr, adults can get them too. The same rules apply: flat rash after day 5? Likely harmless. Raised, itchy rash within hours? Stop the drug and get help. The risk of mislabeling is just as high in adults-and the consequences are just as serious.
What should I tell my doctor about a past rash?
Be specific. Say: ‘I got a flat, non-itchy rash on day 7 of amoxicillin when I was 5. I finished the course and had no other reactions.’ Don’t say ‘I’m allergic to penicillin.’ That label sticks. Accurate details help your doctor make safer choices. If you’re unsure, ask if you should be tested.
Are there new tests or tools to help with diagnosis?
Yes. The FDA-approved PENtest gives results in 15 minutes. Some hospitals are using AI apps that analyze photos of rashes to tell the difference between allergic and non-allergic types-early versions are 89% accurate. These tools are becoming more common and could soon be part of routine care.
Antibiotics save lives. Misunderstanding rashes can cost them. Know the difference. Ask questions. Trust your doctor-but don’t be afraid to ask for proof.


I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.