When you walk into a pharmacy and pick up a generic version of a branded pill, you’re benefiting from a decades-old legal balance designed to keep drug prices low. But that balance is under constant pressure. Antitrust laws in the pharmaceutical industry aren’t just about stopping monopolies-they’re about making sure generic drugs can actually reach the market when they’re supposed to. And too often, they don’t.
The Hatch-Waxman Act: The Original Deal
In 1984, Congress passed the Drug Price Competition and Patent Term Restoration Act-better known as the Hatch-Waxman Act. It was meant to be a compromise. Branded drug companies got extended patent life to reward innovation. Generic manufacturers got a faster, cheaper path to market through the Abbreviated New Drug Application (ANDA). But there was a catch: the first generic company to challenge a patent with a Paragraph IV certification got 180 days of exclusive rights to sell the generic version.
This exclusivity wasn’t a reward-it was a tool. It gave the first generic entrant the power to slash prices and force others to follow. By 2016, generic drugs accounted for 90% of all prescriptions filled in the U.S., up from just 19% in 1984. Between 2005 and 2014, they saved consumers $1.68 trillion. In 2012 alone, that number hit $217 billion.
But the system only works if the first generic actually shows up. And sometimes, they never do.
Pay-for-Delay: The Hidden Tax on Patients
One of the most damaging tricks in the playbook is called "pay-for-delay." That’s when a brand-name drugmaker pays a generic company to stay off the market. It sounds like a bribe-and legally, it often is.
The Supreme Court ruled in FTC v. Actavis (2013) that these deals can violate antitrust laws if they involve large, unexplained payments. The logic is simple: if a generic company could win a patent challenge and make millions by selling cheap drugs, why would it accept millions from the brand to wait? Unless someone’s paying it to stay quiet.
One of the biggest examples came from Gilead Sciences. In 2023, the company paid $246.8 million to settle claims it blocked generic versions of its HIV drug Truvada. The FTC had been investigating for years. Patients waited. Prices stayed high. Lives were affected.
The FTC has brought 18 pay-for-delay cases since 2000. Settlements totaled over $1.2 billion. But for every case settled, dozens more go unnoticed. These aren’t just legal technicalities-they’re direct hits to people’s wallets and health.
Product Hopping and Patent Games
Another tactic? Product hopping. That’s when a drugmaker makes a tiny change to its branded drug-say, switching from a pill to a capsule-right before the patent expires. Then they market the new version as "improved," even if it’s not clinically better.
AstraZeneca did this with Prilosec and Nexium. Prilosec’s patent was about to expire. Nexium came out with a slightly different chemical structure. Doctors were told it was more effective. Patients were switched. Generic Prilosec was blocked from replacing it. Courts eventually dismissed claims that this was illegal monopolization-but the effect was clear: patients paid more, longer.
The FTC calls this a "sham" strategy. It doesn’t innovate. It delays. And it’s still happening. In 2023, the agency sued Teva Pharmaceuticals for using fake citizen petitions to delay generic competition for its multiple sclerosis drug Copaxone. The case is still pending.

Orange Book Abuse and Sham Petitions
The FDA’s Orange Book lists every patent tied to a branded drug. Generic manufacturers must certify against each one. If they say a patent is invalid or not infringed, they trigger a 30-month delay on generic approval-unless they win in court.
Some companies abuse this. They list patents that have nothing to do with the drug’s chemistry. They file patents on packaging, dosage forms, or methods of use that don’t even block generic production. The FTC called this out in its 2003 case against Bristol-Myers Squibb, which listed patents for a drug delivery system that didn’t prevent generic copies.
Then there are sham citizen petitions. These are formal complaints filed with the FDA, claiming a generic drug is unsafe or ineffective. Often, they’re written by lawyers, not scientists. They have no real basis. But they trigger delays. And delays mean higher prices.
Global Differences: What Happens Elsewhere
The U.S. isn’t alone in fighting these tactics-but it’s not always the strictest.
In the European Union, regulators focus on regulatory manipulation. Companies withdraw marketing authorizations in certain countries to block generics from entering. They mislead patent offices to extend protection. The European Commission found that delays in generic entry cost European consumers €11.9 billion every year.
China moved fast in 2025, releasing new Antitrust Guidelines for the Pharmaceutical Sector. They identified five "hardcore restrictions"-price fixing, market division, output limits, joint boycotts, and blocking new technology. By Q1 2025, six cases had been penalized, five involving price-fixing through messaging apps and algorithms. Chinese regulators are now using AI to monitor online pricing collusion in real time.
The U.S. still leads in enforcement volume, but other regions are catching up. And the tactics are evolving.
Who Pays the Price?
Behind every delay in generic entry is a real person.
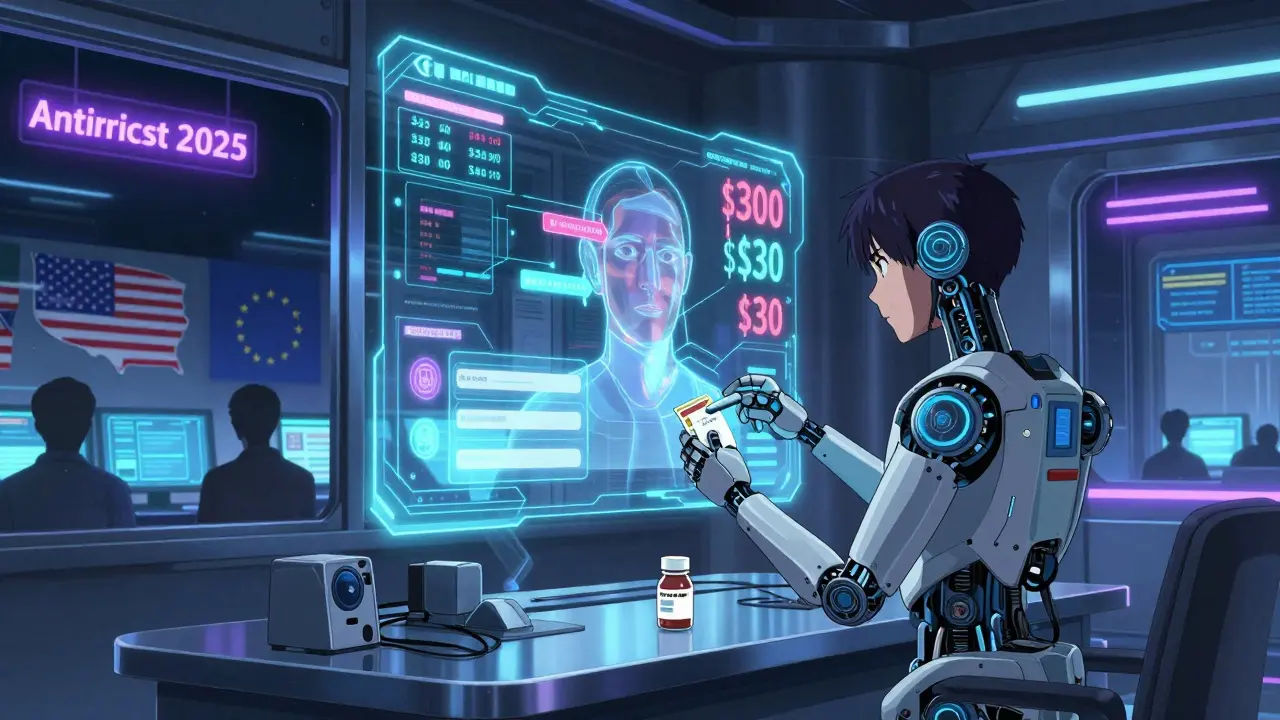
A 2022 Kaiser Family Foundation survey found that 29% of U.S. adults skipped or cut doses of their medication because they couldn’t afford it. That’s not just about income. It’s about access. When a generic drug is blocked for six months, a patient might pay $300 a month instead of $30. That’s $1,800 in extra cost. For someone on a fixed income, that’s food or rent.
Generic drugs cut prices by 30% to 90% compared to branded versions. That’s not a guess. It’s what the Congressional Budget Office documented. When five generic makers enter the market, prices drop nearly 85% from the original brand price. That’s the power of competition.
But when antitrust laws are weakened-or ignored-those savings vanish.
What’s Next?
Antitrust enforcement in generic drug markets is no longer just about big mergers or price fixing. It’s about subtle, legal loopholes that keep prices high. The tools are there: the Hatch-Waxman Act, the FTC, the courts. But they need to be used.
Patients don’t need more studies. They need faster approvals. They need fewer delays. They need regulators who won’t let companies game the system.
The next time you fill a prescription and see "generic" on the label, remember: that’s not luck. It’s the result of laws, lawsuits, and pressure from agencies fighting to keep competition alive. But that fight is far from over.
What is the Hatch-Waxman Act and how does it affect generic drugs?
The Hatch-Waxman Act of 1984 created a legal pathway for generic drug manufacturers to bring cheaper versions of branded drugs to market without repeating expensive clinical trials. It gives the first generic company to challenge a patent with a Paragraph IV certification 180 days of market exclusivity. This system has enabled generics to make up 90% of U.S. prescriptions today, saving consumers over $1.6 trillion since 2005.
What is a "pay-for-delay" agreement in the pharmaceutical industry?
A "pay-for-delay" agreement happens when a brand-name drug company pays a generic manufacturer to delay launching its cheaper version. These deals keep prices high and block competition. The Supreme Court ruled in 2013 that such agreements can violate antitrust laws if they involve large, unexplained payments. Gilead Sciences paid $246.8 million in 2023 to settle one such case involving its HIV drug Truvada.
How do companies use the Orange Book to block generic drugs?
The FDA’s Orange Book lists patents tied to branded drugs. Generic companies must certify against each patent. Some brand companies abuse this by listing weak or irrelevant patents-like those covering packaging or delivery methods-to trigger automatic 30-month delays in generic approval. The FTC has taken action against companies like Bristol-Myers Squibb for this practice, calling it anti-competitive.
What is "product hopping" and why is it controversial?
Product hopping is when a drugmaker makes a minor, often meaningless change to its branded drug-like switching from a pill to a capsule-right before the patent expires. They then push doctors and patients to switch to the new version, making the old one ineligible for generic substitution. AstraZeneca did this with Prilosec and Nexium. Courts have often dismissed these cases as legal, but critics say it’s a tactic to extend monopoly pricing.
How do antitrust laws in China differ from those in the U.S.?
China’s 2025 Antitrust Guidelines for the Pharmaceutical Sector explicitly ban price fixing, market division, and blocking new technology. They’ve already penalized six cases, five of which involved price-fixing through messaging apps and algorithms. Unlike the U.S., which focuses on pay-for-delay and patent abuse, China is using AI to detect online collusion and is cracking down harder on direct price agreements between manufacturers.
Why do generic drugs save so much money?
Generic drugs don’t need to repeat expensive clinical trials because they prove bioequivalence to the brand-name version. Once competition kicks in, prices drop by 30% to 90%. With five generic makers, prices fall nearly 85% from the original brand price. The Congressional Budget Office confirms these savings are real and substantial-often saving patients hundreds or thousands per year.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.