When you’ve got a throbbing headache, a sore back, or swollen knees, you reach for the medicine cabinet. But do you grab ibuprofen or Tylenol? It’s not just a matter of preference-it’s about what’s actually happening in your body. NSAIDs and acetaminophen both ease pain, but they work in completely different ways. Choosing the wrong one could mean less relief-or worse, harm.
How NSAIDs Really Work
NSAIDs-like ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin-don’t just mask pain. They fight inflammation at the source. These drugs block enzymes called COX-1 and COX-2, which your body uses to make prostaglandins. Prostaglandins cause swelling, heat, and pain when you’re injured. So when you take an NSAID for a sprained ankle or arthritis flare-up, you’re not just numbing the ache-you’re calming the inflammation that’s causing it.
That’s why NSAIDs are the go-to for conditions where swelling is part of the problem: tendonitis, muscle strains, menstrual cramps, and osteoarthritis. A 2023 review from the Hospital for Special Surgery found that people with knee or hip osteoarthritis get significantly better pain control with NSAIDs than with acetaminophen alone. If your pain comes with redness, warmth, or stiffness, NSAIDs are likely your best bet.
But there’s a cost. By blocking COX-1, NSAIDs also reduce the protective mucus lining in your stomach. That’s why about 1 in 5 regular users end up with stomach irritation, ulcers, or bleeding. The risk goes up with age, alcohol use, or taking them for more than a few days. Long-term use also raises the chance of heart attack or stroke, especially at higher doses. The FDA has required black box warnings on all NSAIDs since 2005 for this reason.
How Acetaminophen Works-And Doesn’t
Acetaminophen, the active ingredient in Tylenol, is a mystery compared to NSAIDs. Scientists still aren’t sure exactly how it blocks pain, but they know it doesn’t touch inflammation. It works mainly in the brain and spinal cord, lowering your pain threshold and reducing fever. That’s why it’s great for headaches, colds, fevers, or minor aches without swelling.
But here’s the catch: if your pain comes from inflammation-like a pulled muscle or arthritic joint-acetaminophen won’t cut it. Studies show it’s significantly less effective than NSAIDs for joint and back pain. A 2023 analysis from Harvard Health says acetaminophen is “easy on the stomach,” and that’s true. It doesn’t irritate your gut like NSAIDs do. For people with ulcers, kidney issues, or who take blood thinners, it’s often the safer first choice.
But there’s another danger-your liver. Acetaminophen is metabolized there. Take more than 4,000 milligrams in a day (that’s eight 500mg tablets), and you risk acute liver failure. The FDA estimates that acetaminophen overdose causes 56,000 ER visits and 425 deaths every year in the U.S. And it’s easy to overdose accidentally. Cold medicines, sleep aids, and prescription painkillers like Vicodin all contain acetaminophen. You might think you’re taking just one Tylenol, but if you’re also taking a cold tablet, you could be hitting 1,500mg without realizing it.
When to Choose Which
It’s not about which is “better.” It’s about which fits your situation.
- Choose NSAIDs if: Your pain comes with swelling-think sprains, arthritis, back pain, or menstrual cramps. Ibuprofen or naproxen will give you real relief by reducing the inflammation.
- Choose acetaminophen if: You have a headache, fever, or general body aches with no swelling. It’s also safer if you have a history of stomach ulcers, are on blood thinners, or have kidney disease.
There’s no point in taking an NSAID for a tension headache-it won’t help more than acetaminophen, but it’ll risk your stomach. And don’t waste acetaminophen on a swollen knee-it won’t reduce the swelling, so the pain will likely come back.
Combining Them: A Smart Strategy
Here’s something most people don’t know: you can take both together-and many doctors recommend it.
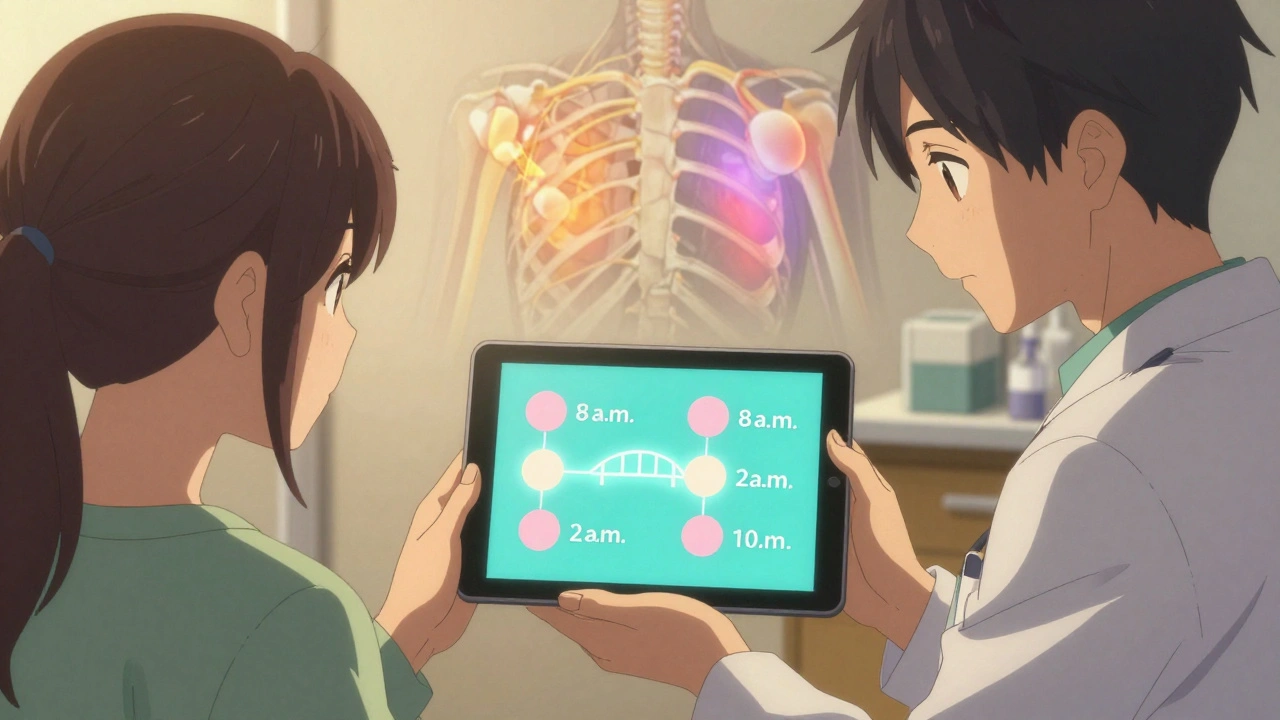
Research from the Hospital for Special Surgery shows that combining low-dose acetaminophen with low-dose ibuprofen gives better pain control than either one alone. For example: take 500mg of acetaminophen at 8 a.m., then 400mg of ibuprofen at 2 p.m., then acetaminophen again at 8 p.m., and ibuprofen at 10 p.m. This keeps pain under control while keeping the daily dose of each drug well below the danger zone.
This approach is especially useful for chronic pain like osteoarthritis. You get the anti-inflammatory power of NSAIDs and the liver-safe, gut-friendly relief of acetaminophen-all with lower total doses. Less risk, more relief.
Safety First: Dosing and Warnings
Overdosing on either drug is easy-and dangerous.
Acetaminophen: Never exceed 3,000mg per day if you drink alcohol, have liver disease, or are over 65. The FDA recommends 3,000mg as the new safe max for most adults, not 4,000mg. Check every medicine you take-cold pills, sleep aids, prescription opioids-all may contain acetaminophen.
NSAIDs: Don’t use them for more than 10 days for pain or 3 days for fever without talking to a doctor. Stick to the lowest effective dose: 200mg ibuprofen every 6 hours, or 220mg naproxen every 12 hours. Avoid if you have high blood pressure, heart disease, or kidney problems.
And never mix NSAIDs. Don’t take ibuprofen and naproxen together. Don’t take aspirin and ibuprofen together if you’re using aspirin for heart protection-ibuprofen can block its benefits.
Who Should Avoid These Medications?
Some people should skip NSAIDs entirely:
- People with stomach ulcers or bleeding disorders
- Those with heart failure, high blood pressure, or kidney disease
- Pregnant women after 20 weeks (NSAIDs can affect fetal circulation)
Acetaminophen isn’t risk-free either:
- People with liver disease or who drink alcohol regularly
- Those taking warfarin (acetaminophen can increase bleeding risk)
- Anyone taking multiple medications that contain acetaminophen
If you’re on any prescription meds, have chronic health issues, or take pain relievers more than a few times a week, talk to your doctor before choosing. What works for your neighbor might not be safe for you.
What the Experts Say
Doctors don’t pick one over the other blindly. They look at the cause of the pain, your medical history, and your risk factors.
Dr. Kramskiy at the Hospital for Special Surgery says: “Tylenol is most effective when taken as part of a regimen with NSAIDs.” That’s not an offhand comment-it’s based on clinical trials showing better outcomes when both are used together.
The American Academy of Family Physicians reminds us that their advice only applies to healthy adults who use pain relievers occasionally. If you’re taking them daily for back pain or arthritis, you need a personalized plan-not a pharmacy aisle decision.
And here’s a practical tip from healthcare providers: if you’re unsure, start with acetaminophen. It’s gentler. If it doesn’t help after a day or two, switch to an NSAID. If you’re still in pain, see your doctor. Don’t keep cranking up the dose.
Bottom Line: Match the Drug to the Problem
NSAIDs fight inflammation. Acetaminophen eases pain and fever. Neither is “stronger”-they’re just different tools.
For swelling? NSAIDs. For headaches or fever? Acetaminophen. For chronic joint pain? Try both, spaced apart. For safety? Stick to the lowest dose, don’t mix, and never exceed daily limits.
Most people don’t realize how easy it is to overdose on acetaminophen-or how risky long-term NSAID use can be. But with the right info, you can use these common drugs safely and effectively. You don’t need to guess. You just need to know what’s causing your pain-and which drug actually targets it.


I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.