When you’re managing a chronic condition like high blood pressure or type 2 diabetes, you’re likely on more than one medication. That’s where combo generics come in - pills that combine two or more drugs in a single tablet. They sound convenient. But are they worth the price?
Here’s the hard truth: in many cases, buying the same drugs as separate generic pills saves you hundreds - sometimes thousands - of dollars a year. And it’s not just a theory. Real data from Medicare shows billions in wasted spending because doctors and pharmacies defaulted to branded combo pills when cheaper alternatives existed.
Why Combo Pills Cost So Much
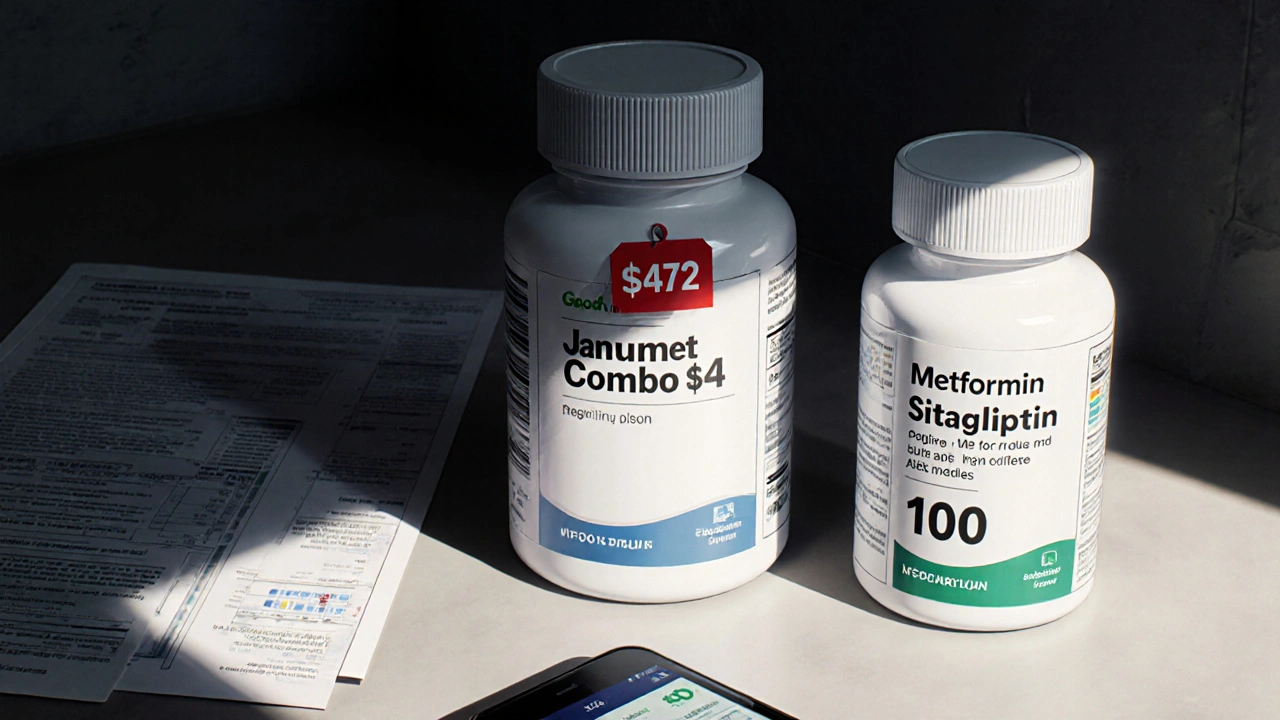
Fixed-dose combinations (FDCs) aren’t new. They’ve been around for decades. But over the last 10 years, drugmakers have used them in a way that’s hard to justify. Take Janumet, a combo of sitagliptin and metformin. In 2016, Medicare paid an average of $472 for a 30-day supply of this branded combo. Meanwhile, generic metformin? At Walmart’s $4 program, it cost $4. The sitagliptin component? Even as a brand, it wasn’t much more than $100 a month. Put them together? You’d expect around $104. But the combo pill? Nearly $472. That’s a 350% markup.
This isn’t rare. A 2018 study in JAMA Internal Medicine looked at 29 branded combo drugs and found Medicare spent $925 million more in 2016 than it would have if patients had taken the same drugs as separate generics. For the 10 most expensive combos, the savings potential was $2.7 billion. That’s not a rounding error. That’s money pulled straight out of the pockets of taxpayers and patients.
Why does this happen? It’s called evergreening. When one drug in a combo loses its patent, the manufacturer pairs it with a new, still-patented drug. Suddenly, the whole combo stays protected. Even if one component is cheap, the combo stays expensive. Nexlizet - a combo of ezetimibe (generic since 2016) and bempedoic acid (new, expensive) - costs over $12 a day in the U.S. That’s $360 a month. Generic ezetimibe alone? About $10. The new drug might cost $150. So why pay $360? Because the combo is still under patent. And insurers often don’t push back.
How Much Can You Actually Save?
Let’s break down real numbers from common combo drugs:
- Entresto (sacubitril/valsartan): $550/month. Generic valsartan? $15. Sacubitril alone? Around $300. Total if bought separately: ~$315. That’s $235 saved per month.
- Kazano (alogliptin/metformin): $425/month. Generic metformin? $4-$10. Alogliptin? ~$200. Separate total: ~$210. Savings: $215/month.
- Januvia + Metformin (separate): $300 + $10 = $310. Janumet (combo): $472. You’re paying $162 extra for the convenience of one pill.
These aren’t outliers. They’re standard. The FDA says generic drugs cost 80-85% less than brand-name versions. But combo pills break that rule. They’re priced like brand-name drugs even when one or both ingredients are generic.
And here’s the kicker: most of these combos are not even the first-line treatment. Metformin, for example, is the gold standard for type 2 diabetes. It’s been used for over 60 years. Yet when paired with a newer drug in a combo, the price skyrockets. Why? Because the system rewards complexity over simplicity.

Who Pays the Price?
It’s not just Medicare. Private insurers, pharmacy benefit managers (PBMs), and patients all foot the bill. In 2021, combo drugs made up just 2.1% of prescriptions but 8.3% of Medicare Part D spending. That means a tiny fraction of pills were eating up nearly one in 10 dollars spent on drugs.
Many Part D plans now require prior authorization for high-cost combos. That’s a red flag. If your insurer has to approve something before you can get it, they already know it’s overpriced. Some plans even have "carve-outs" - they won’t cover the combo at all unless you prove you’ve tried the separate generics first.
Patients don’t always know this is an option. Doctors don’t always bring it up. And pharmacies? They’re often paid more to dispense the combo pill because it’s branded. It’s not that they’re being dishonest - they’re just following the system. But that system is broken.
Is Convenience Worth the Cost?
Drug companies argue that combos improve adherence. Take a study from the American College of Cardiology: patients on combo pills were 25% more likely to stick with their treatment than those on multiple pills. That’s real. Skipping pills can lead to hospitalizations, which cost far more than any drug.
But here’s the problem: that benefit doesn’t justify a 300% price hike. If you’re paying $500 a month for a combo, you’re already struggling. Many patients cut pills in half or skip doses because they can’t afford it. If you can get the same drugs for $100 a month, you’re far more likely to take them consistently.
And if adherence is the goal, there are better tools. Pill organizers, smartphone reminders, and once-daily generics exist. You don’t need a fancy combo pill to stay on track. You need affordable access.
What You Can Do
You’re not powerless. Here’s how to take control:
- Ask your doctor: "Are there generic versions of each of these drugs? Can I take them separately?" Don’t assume the combo is the only option.
- Check prices: Use GoodRx or your pharmacy’s price checker. Compare the combo to the sum of the individual generics. You’ll often be shocked.
- Request a prior authorization exception: If your plan denies the combo, ask for a form to appeal based on cost. Many plans will approve the generics if you show the price difference.
- Use mail-order pharmacies: Some offer deeper discounts on generics. A 90-day supply of metformin might cost $15 instead of $10 for 30 days.
- Look for manufacturer assistance: Some companies offer co-pay cards. Novartis’s Entresto Access Program cuts the price to $10 for eligible Medicare patients. That’s helpful - but still $90 more than generics.
Don’t feel guilty for asking. This isn’t about being cheap. It’s about getting the same clinical outcome without paying a premium for packaging.
The Bigger Picture
This isn’t just about your prescription. It’s about how the system works. The Inflation Reduction Act of 2022 gave Medicare the power to negotiate drug prices - and combo drugs are high on the list. The Congressional Budget Office predicts Medicare will spend an extra $14.3 billion on these overpriced combos between 2023 and 2032.
Regulators are starting to notice. The FDA is pushing to speed up generic approvals. The Medicare Payment Advisory Commission has called for payment changes that reflect the true cost of combo drugs. But change moves slowly.
Until then, the best tool you have is information. Know the prices. Ask the questions. Push back when it makes sense. You’re not just saving money - you’re pushing back on a system that’s designed to make you pay more for less.
There’s no magic pill. But there is a smarter way to get the same treatment - and it doesn’t cost a fortune.

I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.