Managing multiple medications can feel overwhelming. You’ve got pills for your blood pressure, your diabetes, your cholesterol, maybe a pain reliever, a vitamin, and something for your sleep. And you’re not sure if you’re taking them at the right time, or if they’re even working the way they should. You’re not alone. Nearly half of people taking chronic medications don’t take them as prescribed. But there’s a simple, powerful tool that can change that: a medication action plan.
What Is a Medication Action Plan?
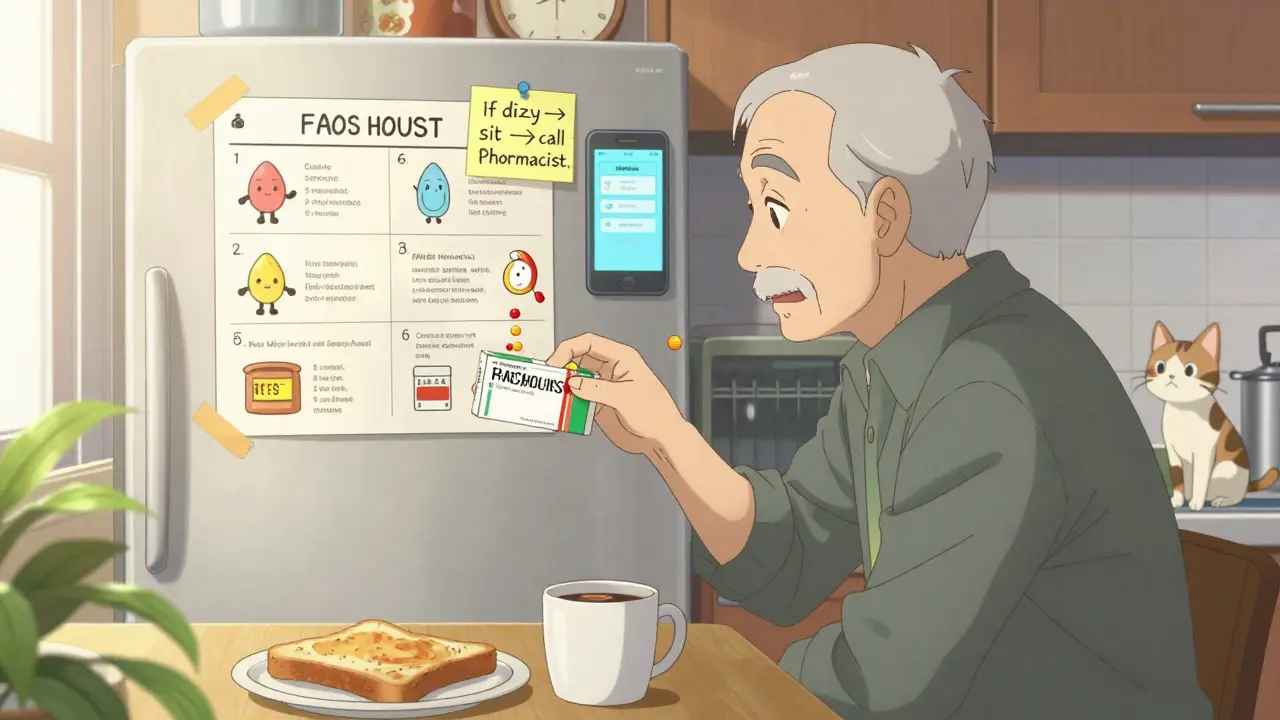
A medication action plan (MAP) isn’t just a list of your drugs. It’s a personalized roadmap - written in plain language - that tells you exactly what to do, when, and why. Think of it as your daily guide to staying healthy while taking your medicines. It answers questions like: Which pill do I take with breakfast? What should I do if I feel dizzy? When should I call my doctor? It’s created with your care team - usually your doctor, pharmacist, and sometimes a nurse or care coordinator. Unlike a generic printout from the pharmacy, a real MAP is built around your life. If you forget pills because you don’t eat breakfast, the plan might say: "Take your morning pill after your coffee." If you’re scared of side effects, it might include a simple checklist: "If you feel faint, sit down and call your pharmacist. Do not drive." These plans are backed by real data. In the U.S., patients who use personalized medication action plans see adherence rates jump by 25% to 40%. Hospital visits due to medication mistakes drop by 32% in the year after getting one. In Germany, since 2016, anyone on three or more prescribed medicines gets a free, standardized plan updated every time they pick up a new prescription.Why Your Care Team Is Key
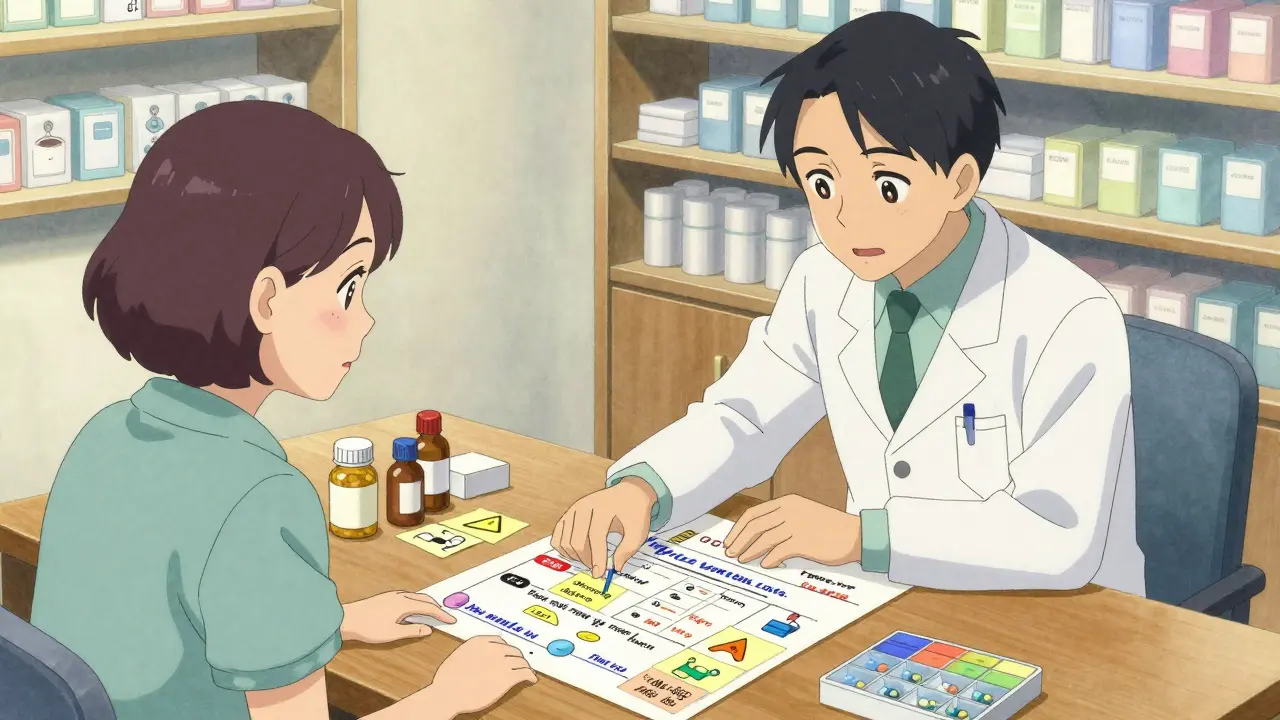
You can’t make a good medication action plan alone. Your doctor knows what you’re treating. Your pharmacist knows how the pills interact, what over-the-counter drugs might clash, and what side effects to watch for. Together, they spot problems you might miss - like taking two different pills that do the same thing, or a vitamin that makes your blood thinner less effective. The best plans are co-created. That means you don’t just get handed a paper. You sit down with your pharmacist or care provider and say: "I usually take my pills at night, but I forget because I’m tired." Or: "I stopped my cholesterol pill because it made me feel sick, but I didn’t know who to ask." That’s when the plan becomes real. In Australia, Medicare and private health insurers increasingly cover medication reviews with pharmacists. You can book a free or low-cost session just to talk through your meds - no appointment needed at many pharmacies. Bring everything you take: prescriptions, supplements, herbal teas, even that aspirin you keep in your wallet.Step-by-Step: How to Build Your Plan
Creating your plan doesn’t take a big appointment. Start here:- Collect everything. Gather all your medications - pills, patches, inhalers, eye drops, vitamins, and even the herbal stuff. Put them in a bag. Don’t leave anything out. Many people forget their painkillers or sleep aids, but those can cause serious problems with other drugs.
- Book a medication review. Call your pharmacy or GP and ask for a Comprehensive Medication Review (CMR). It’s usually free under Medicare if you take 5 or more chronic meds. The session lasts 30 to 60 minutes.
- Ask the big questions. During your review, say: "Why am I taking each of these?" "What happens if I miss one?" "Is there a cheaper or simpler way?" Write down their answers.
- Build your action steps. Work with your pharmacist to turn each problem into a clear action. Example: Instead of "Take metformin daily," write "Take 500mg with breakfast, every day. If you skip breakfast, take it with lunch. If you feel nauseous, call me."
- Make it visual. Use color codes, pictures, or sticky notes. One patient in Melbourne stuck photos of her pills next to her coffee mug and dinner plate. Her adherence jumped from 65% to 95%.
- Get a copy. Ask for a printed version. Save a digital copy on your phone. Give one to a family member or caregiver.
What Should Be in Your Plan?
A good medication action plan includes these six things:- A full list of every medicine you take - including dose, frequency, and why you take it.
- Clear instructions for each pill: when to take it, with or without food, what to avoid.
- Warning signs - what symptoms mean you should call someone. Example: "If your leg swells suddenly, call your doctor immediately - it could be a blood clot."
- What to do if you miss a dose - not just "take it later," but specific rules like "If you forget your evening blood pressure pill after 8 p.m., skip it. Don’t double up."
- Goals - measurable targets like: "Take all morning pills for 7 days straight," or "Reduce my pain from 7/10 to 4/10 in 4 weeks."
- Contact info - who to call for questions: your pharmacist, your doctor, or a 24/7 helpline.
Common Mistakes to Avoid
Many people get a plan - but it doesn’t help. Why? Here’s what goes wrong:- Too generic. Pre-printed templates with no personalization don’t work. If the plan says "Take medication daily," but you work nights, it’s useless.
- Too medical. Words like "hypertension," "polypharmacy," or "adherence" confuse people. Use "high blood pressure," "taking too many pills," and "remembering to take them."
- Not updated. Your plan should change when your meds change. If your doctor adds a new pill or stops one, get the plan revised - don’t just scribble it in.
- Hidden away. If it’s stuck in a drawer, it won’t help. Keep it on your fridge, in your wallet, or as a saved photo on your phone.
Real Success Stories
One 72-year-old man in Ballarat was taking 11 different medications. He didn’t know why he took half of them. After a 45-minute session with his pharmacist, his plan was simplified to 6 essential pills. Each had a clear reason: "This one lowers your heart rate," "This one stops your kidneys from getting damaged." He started using a pill box with alarms. Within 3 months, his blood pressure dropped into the normal range - and he hadn’t been to the hospital in over a year. Another woman with type 2 diabetes kept forgetting her insulin. Her plan didn’t say "Inject insulin before meals." Instead, it said: "Put your pen next to your fork. Take it right before you eat your main meal. If you’re out, call your daughter - she’ll remind you." She started carrying her insulin with her lunch bag. Her A1C dropped from 8.9 to 6.7.What If You Can’t Get a Plan?
Not everyone gets one automatically. If your doctor or pharmacist hasn’t offered you a medication action plan, ask for one. Say: "I’m taking several medications and want to make sure I’m doing it right. Can we make a simple plan together?" If you’re on Medicare Part D (or have private insurance), you’re likely eligible for a free medication review. Check your insurer’s website or call their member services. Even if you’re not on Medicare, many community pharmacies offer low-cost reviews. If you’re helping an elderly parent or someone with memory issues, go with them. Bring a notebook. Ask questions. Take notes. You’re not just helping - you’re preventing a hospital trip.Keeping Your Plan Alive
Your plan isn’t a one-time thing. Treat it like a living document:- Review it every 3 months - or anytime your meds change.
- Update it when you start or stop anything - even a new supplement or painkiller from the pharmacy.
- Ask yourself every month: "Am I taking my pills like the plan says?" If not, why? Is it too complicated? Too expensive? Too confusing?
- Share it with anyone who helps you - family, carers, nurses.
Final Thought: Your Health, Your Plan
You’re not just a patient. You’re the most important person in your care team. A medication action plan isn’t about following rules - it’s about giving you control. It turns confusion into clarity. Fear into confidence. And forgetfulness into consistency. Start small. Bring your meds to the pharmacy this week. Ask for a review. Say: "I want to take my pills right - can we make a plan that actually works for me?" That’s all it takes.What’s the difference between a medication list and a medication action plan?
A medication list just shows what drugs you take - name, dose, frequency. A medication action plan goes further. It tells you why you take each one, what to do if you miss a dose, what side effects to watch for, and how to adjust based on your daily life. It’s a guide, not just a record.
Can I make a medication action plan myself?
You can start one, but it won’t be complete or safe without your care team. Pharmacists and doctors spot dangerous interactions, unnecessary duplicates, and dosage errors you might miss. A plan made alone might look good on paper, but it could put you at risk. Always get professional input before acting on it.
Do I need to pay for a medication action plan?
No - if you’re eligible, it’s free. In Australia, Medicare covers Comprehensive Medication Reviews for people taking 5 or more chronic medications. Many private insurers and community pharmacies offer them at no cost. Ask your pharmacist: "Is this service covered under my plan?" If they say no, ask why - and request a referral.
What if I don’t understand the medical terms on my plan?
Say so. Right away. Your care team is there to help you understand - not to use jargon. Ask them to rewrite any confusing parts in plain English. Example: Replace "hypertension" with "high blood pressure," or "polypharmacy" with "taking too many medicines." A good plan uses your words, not the textbook.
How often should I update my medication action plan?
Update it every time your medications change - whether it’s a new prescription, a dose change, or you stop taking something. Even if nothing changes, review it every 3 months. Your body, your routine, and your needs change. Your plan should too.
Can my family help with my medication action plan?
Yes - and they should. Give a copy to a trusted family member or caregiver. They can help you remember doses, spot side effects, or call your pharmacist if something feels off. Many successful plans include a "who to call" section with names and numbers. You’re not alone - let your team help.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.