Most people think when a drug’s patent expires, generics can jump in and slash prices. That’s not how it works anymore. In reality, the clock doesn’t start ticking on generic competition when the patent runs out-it often starts years later, thanks to a complex web of market exclusivity extensions. These aren’t patents. They’re regulatory tricks built into U.S. and EU law that let drugmakers delay generics long after the original patent has expired. And they’re costing patients and insurers billions every year.
How Market Exclusivity Works-Without a Patent
Patents give inventors 20 years of protection from the day they file. But for drugs, that clock starts ticking long before the product hits shelves. By the time a drug gets FDA approval, five to ten years may have already passed in clinical trials. That leaves little time to recoup the $2.3 billion average cost of development. So Congress created regulatory exclusivities-separate from patents-to give companies extra time to profit without competition. These aren’t loopholes. They’re legal tools written into the Hatch-Waxman Act of 1984. The idea was simple: reward innovation, but let generics in eventually. Today, that balance is broken. Companies now stack multiple exclusivities like layers of armor. One drug can have patent term extensions, orphan drug status, pediatric add-ons, and new indication protections-all running at once.The Five Main Exclusivity Types in the U.S.
The FDA offers five key types of market exclusivity, each with its own rules:- New Chemical Entity (NCE) exclusivity: Five years of protection for a drug with a completely new active ingredient. During this time, the FDA can’t even accept a generic application.
- Orphan Drug exclusivity: Seven years for drugs treating diseases affecting fewer than 200,000 Americans. This is a lifeline for rare disease treatments-but also a magnet for companies targeting niche markets with high prices.
- New Clinical Investigation exclusivity: Three years for a new use, dosage, or formulation of an existing drug. To qualify, you must prove the new version offers real clinical benefits, not just convenience.
- Pediatric exclusivity: Six months added to any existing exclusivity period if the company completes FDA-requested pediatric studies. This isn’t optional-it’s a financial incentive. For blockbuster drugs, six months can mean over $1 billion in extra revenue.
- Patent challenge exclusivity: 180 days of exclusive rights for the first generic company to challenge a patent successfully. This is the only exclusivity meant to speed up generics, not delay them.
Here’s the catch: these exclusivities can stack. A drug might get five years of NCE protection, then six more months for pediatric studies, then three more years for a new use. That’s 8.5 years before generics can even apply. Add patent extensions on top, and you’re looking at a decade or more of monopoly pricing.
How the EU Does It Differently
The European Union doesn’t use the same system. Instead of multiple exclusivity types, they rely on the Supplemental Protection Certificate (SPC). An SPC can extend market protection up to 15 years after the drug’s first approval in the EU-sometimes longer if pediatric studies are completed. EU orphan drug exclusivity lasts 10 years, with a two-year extension for pediatric data. That’s longer than the U.S. version. But unlike the U.S., the EU doesn’t let companies stack multiple exclusivities on the same drug. One exclusivity applies at a time. That sounds fairer-but it also means companies there focus more on maximizing the SPC rather than juggling layers of protection. Still, both systems end up with the same result: patients wait longer for cheaper drugs.
The Patent Thicket Strategy
Patents aren’t dead-they’re just not the only weapon. Companies now file dozens of secondary patents on tiny changes: a new pill coating, a slightly different dosage form, a new delivery device. These aren’t breakthroughs. They’re tweaks. Take tazarotene, a skin treatment. Its core patent expired years ago. But the company filed 48 additional patents covering everything from packaging to application methods. Each one delays a generic. This is called a patent thicket. It’s not illegal. It’s strategic. The FDA can’t block these patents. They’re approved by the USPTO, which doesn’t evaluate medical value-only novelty and non-obviousness. So a company can patent a blue pill instead of a white one and legally block generics for years.Product Hopping and the FDA’s Slow Response
Another tactic: product hopping. When a patent is about to expire, a company launches a slightly modified version of the drug-maybe a pill that dissolves faster or a new brand name-and then stops making the original. Prescribers switch. Patients get stuck on the new version. Generics can’t enter because the old drug is gone, and the new one is protected by its own patent or exclusivity. Teva Pharmaceuticals reported in 2022 that this tactic delayed generic entry for 17% of their target drugs. The FTC called it anticompetitive. In 2023, they filed legal briefs arguing it violates antitrust laws. But courts move slowly. Meanwhile, patients pay more.Who Benefits-and Who Pays
The math is brutal. In 2022, branded drugs made up just 10% of prescriptions but 78% of U.S. pharmaceutical spending. Why? Because exclusivity keeps prices high. A 2023 JAMA Health Forum study looked at just four drugs: bimatoprost, celecoxib, glatiramer, and imatinib. When generics finally entered, the extra spending caused by delayed competition totaled $3.5 billion over two years. That’s not inflation. That’s exclusivity. Meanwhile, orphan drug approvals have exploded-from 201 in 2010 to over 1,000 in 2022. That’s good for rare disease patients. But many of these drugs cost over $500,000 a year. And because they get seven to twelve years of exclusivity, there’s little pressure to lower prices.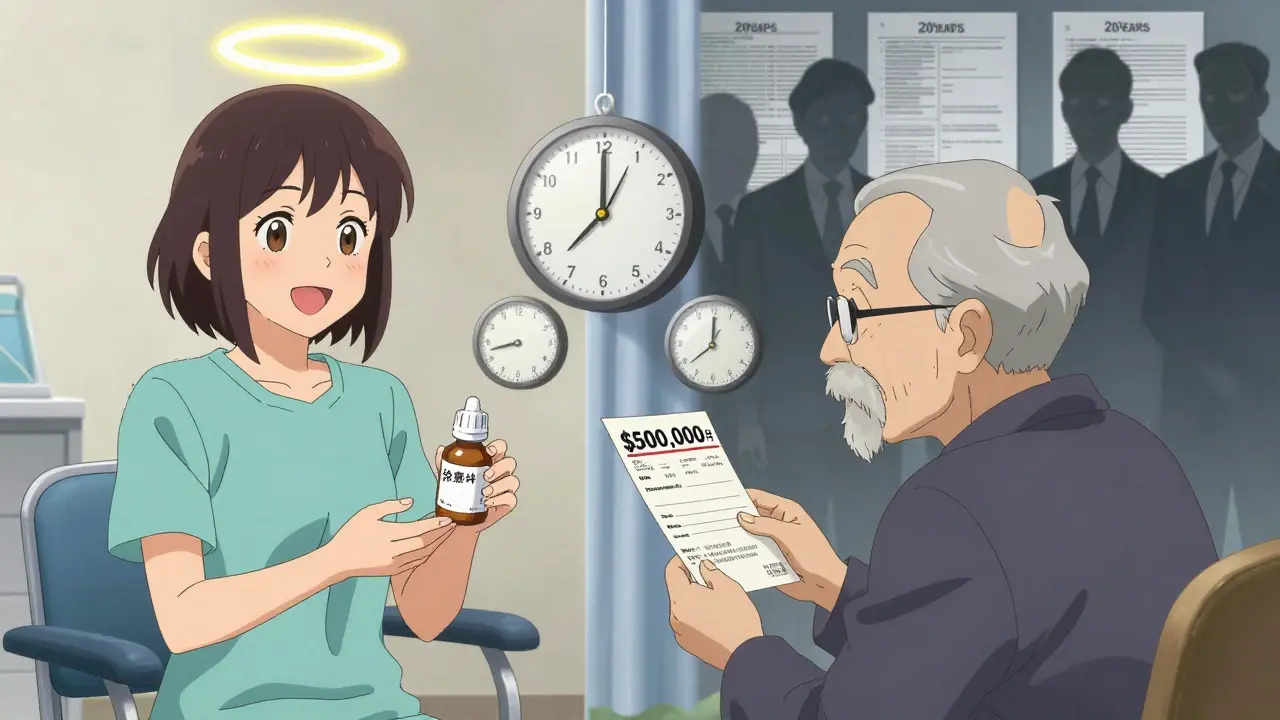
How Companies Play the System
Big pharma doesn’t leave this to chance. They have teams of 15 to 25 specialists-patent lawyers, regulatory experts, clinical strategists-dedicated to managing exclusivity. They start planning during Phase II trials, not after approval. Some delay patent filings until after clinical data is solid, squeezing more years of protection out of the 20-year clock. Others wait for the FDA to request pediatric studies, then complete them just to snag the six-month bonus. One senior patent attorney on Reddit said, “The real art is in stacking exclusivities-getting that pediatric extension can be worth billions.” And it works. For drugs like Vertex’s cystic fibrosis treatments, effective market exclusivity stretches beyond 20 years. That’s not innovation. That’s a legal monopoly.What’s Changing-and What’s Not
Regulators are starting to push back. In 2023, the FDA tightened rules for three-year new indication exclusivity. Now, companies must prove real clinical benefit-not just a different way to take the pill. The European Commission proposed reforming SPCs to reward true innovation, not minor tweaks. But change is slow. The Biotechnology Innovation Organization says 68% of biotech startups need exclusivity to attract funding. Patient groups say orphan drug protections save lives. Both are true. The problem isn’t the intent-it’s the abuse. The average effective exclusivity period for new drugs has jumped from 12.7 years in 2018 to 16.3 years by 2028, according to Evaluate Pharma. That’s nearly double the original 20-year patent term.What This Means for Patients
If you’re taking a brand-name drug, you’re probably paying more than you need to. If your doctor prescribes a new version of an old drug, ask: is this really better-or just newer? If your insurance denies a generic, check if the original is still under exclusivity. There’s no easy fix. But understanding these mechanisms helps. You’re not just buying medicine. You’re paying for legal strategy.Are market exclusivity extensions the same as patents?
No. Patents are intellectual property rights granted by the USPTO. Market exclusivity extensions are regulatory protections granted by the FDA or EMA. You can have exclusivity without a patent, and vice versa. For example, an orphan drug might have seven years of exclusivity even if no patent exists.
Can a drug have multiple exclusivities at the same time?
In the U.S., yes. A drug can have NCE exclusivity (5 years), pediatric exclusivity (6 months), and new indication exclusivity (3 years) all running together. This stacking is common and legal. In the EU, only one exclusivity applies at a time, though SPCs can be extended with pediatric data.
How long does pediatric exclusivity last?
Six months. But it’s added to whatever exclusivity the drug already has. So if a drug has five years of NCE exclusivity, adding pediatric exclusivity extends it to 5.5 years. For a drug with a patent extension, that six months can mean billions in extra revenue.
Why do companies file so many secondary patents?
To create a patent thicket. Each patent covers a small change-like a new pill shape or delivery method-that doesn’t improve effectiveness but blocks generics. The USPTO approves them based on technical novelty, not medical value. Tazarotene has 48 secondary patents. That’s not innovation. That’s legal defense.
Do market exclusivity extensions help innovation?
They help fund development for risky or niche drugs, especially orphan drugs. But for most blockbuster drugs, they’re used to extend monopolies, not drive innovation. Studies show that 91% of drugs with patent extensions keep their monopolies far beyond the legal limit, mostly through stacking exclusivities, not new science.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.