When you open your medicine cabinet and see a recall notice on the news, your first thought might be to toss the bottle or stop taking it right away. That’s the worst thing you can do. Most medication recalls aren’t emergencies - but they are urgent. And knowing exactly what to do next can keep you safe, avoid dangerous side effects, and prevent unnecessary panic.
Understand the Recall Level - Not All Recalls Are the Same
The FDA classifies drug recalls into three levels based on risk. This isn’t just bureaucracy - it tells you how fast you need to act.- Class I: Highest risk. The drug could cause serious harm or death. These make up about 15% of all recalls. Examples include contaminated blood pressure meds like valsartan or insulin with incorrect dosing.
- Class II: Moderate risk. The drug might cause temporary health issues or reversible side effects. This is the most common type - about 70% of recalls fall here. Think wrong label, missing instructions, or packaging that could lead to confusion.
- Class III: Lowest risk. The drug won’t hurt you, but it breaks a regulation - maybe the expiration date is smudged or the bottle color is off. These are mostly paperwork fixes.
Here’s the key: Only Class I recalls require immediate action. Even then, you don’t stop your medicine cold. You check, you call, you replace - not quit.
Don’t Stop Taking Your Medicine - Check the Lot Number First
The biggest mistake patients make? Stopping their medication because they heard “there’s a recall.” That’s dangerous. If you’re on blood pressure pills, insulin, seizure meds, or antidepressants, stopping suddenly can trigger strokes, seizures, or severe withdrawal.Recalls don’t affect every bottle. Only specific batches - called lots - are recalled. Each bottle has a lot number and expiration date printed on it. Your medication might be perfectly safe, even if others in the same drug class are not.
Here’s how to check:
- Find the lot number on your pill bottle or blister pack. It’s usually a mix of letters and numbers - like “L23AB78” or “2024-09-15.”
- Go to the FDA’s Drug Recalls page at fda.gov/drugs/drug-safety-and-availability/drug-recalls.
- Search by your drug’s brand or generic name. Then filter by “Product Type: Human Drug.”
- Click on the recall notice and compare the lot numbers listed to yours.
If your lot number matches, you’re affected. If it doesn’t? You’re fine. Keep taking your medicine. About 45% of patients assume all lots are recalled - but the FDA says only 10-20% are actually affected in most cases.
Call Your Pharmacy - They’re Your First Line of Defense
Pharmacists are trained to handle recalls. In fact, 92% of U.S. pharmacies have a built-in system to flag recalled drugs as soon as the FDA announces them.Don’t wait. Call your pharmacy the same day you see a recall notice. Give them:
- Your full name
- Your date of birth
- The name of the medication
- The lot number from your bottle
They’ll check their inventory and tell you if your exact bottle is affected. If it is, they’ll usually:
- Give you a replacement from a safe lot within 24 hours
- Send a new prescription to your preferred pharmacy
- Arrange for a different drug if needed - and coordinate with your doctor
Pharmacies can even help you get free replacements if your insurance won’t cover it. Don’t try to figure this out alone. Your pharmacist has direct access to manufacturer data and recall databases you can’t see.

Dispose of Recalled Medication the Right Way
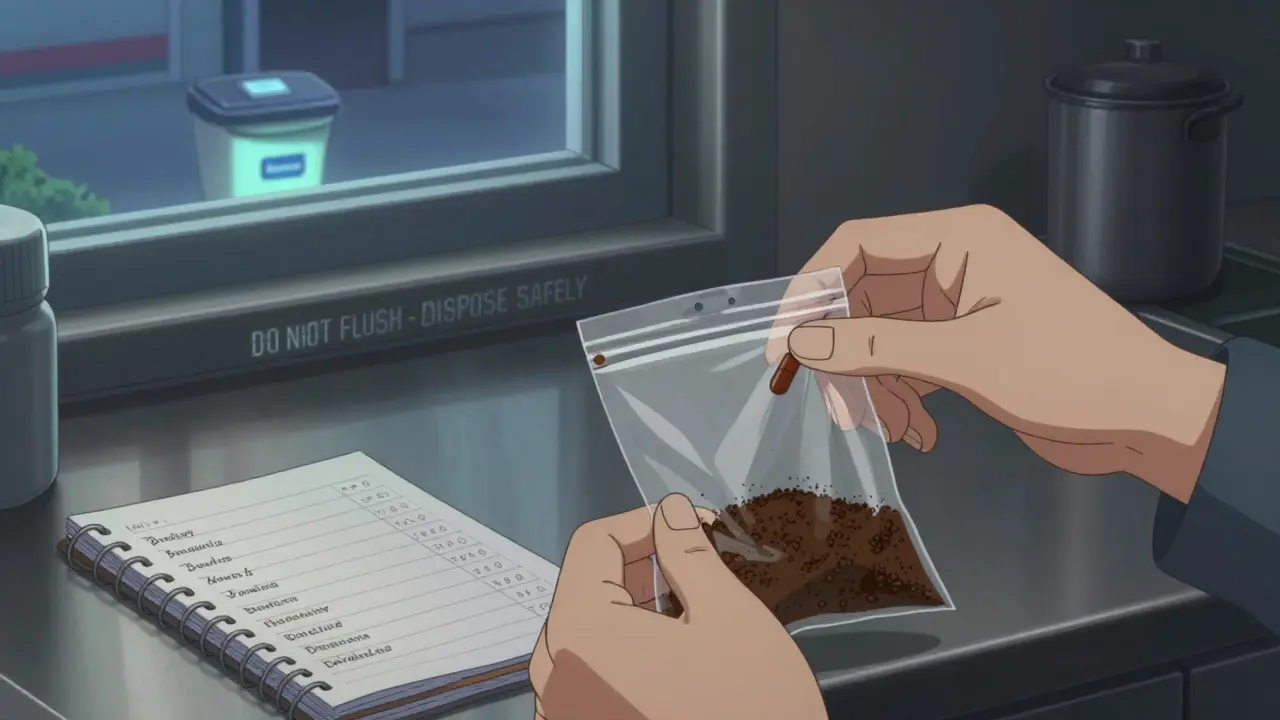
If your pharmacy tells you to throw it out, don’t just toss it in the trash or flush it. That’s harmful to the environment and dangerous for kids or pets.Here’s the safe method:
- Take the pills out of the bottle.
- Mix them with something unappetizing - used coffee grounds, cat litter, or dirt.
- Put the mixture in a sealed plastic bag or container.
- Throw it in the regular trash.
Never flush medications unless the label says to. The FDA says less than 1% of drugs need flushing - mostly opioids with high abuse risk. For everything else, the coffee grounds trick works.
Some pharmacies offer take-back bins. Ask yours if they have one. In Melbourne, many community pharmacies have drop-off boxes for unused or recalled meds.
Watch for Symptoms - And Report Them
Even if you took a recalled drug for only a few days, pay attention to your body. Some side effects show up slowly.Call your doctor immediately if you notice:
- Unusual dizziness, nausea, or vomiting
- Changes in heart rate or breathing
- Skin rashes, swelling, or bruising
- Worsening of your condition (e.g., higher blood pressure, more seizures)
Keep a simple log: write down what you took, when, and any symptoms. This helps your doctor decide if you need tests or a different treatment.
Also, report it to the FDA’s MedWatch program. In 2022, 27% of new recalls started because patients reported strange side effects. Your report could prevent someone else from getting hurt.
What Not to Do - Common Mistakes That Put You at Risk
Here are the top three mistakes patients make during recalls - and why they’re dangerous:- Mistake 1: Stopping your medicine without talking to a provider. In 22% of cases, patients quit cold turkey. That led to hospitalizations for heart failure, seizures, and diabetic ketoacidosis.
- Mistake 2: Assuming all bottles are recalled. 45% of people think if one bottle is bad, all are. But recalls target specific lots. Your bottle might be fine.
- Mistake 3: Throwing pills in the trash or flushing them. 30% of people dispose of meds this way. It pollutes water and risks accidental poisoning.
Remember: A recall doesn’t mean your medicine is poison. It means there’s a fix - and your pharmacist knows how to get it to you.
Prevent Future Problems - Keep a Medication Log
The fastest way to handle a recall is to be ready before it happens.Take five minutes now to create a simple log:
- Drug name (brand and generic)
- Dosage (e.g., 10mg, 2x daily)
- Lot number and expiration date
- Pharmacy name and phone number
Keep it on your phone or in a notebook. People who do this resolve recall issues 60% faster than those who don’t.
Set a reminder every three months to update your list. When you refill a prescription, write down the new lot number. It takes 30 seconds - and could save your life.
What’s Changing in 2026 - And How It Helps You
The FDA is rolling out new systems to reach patients faster. Starting in early 2025, pharmacy benefit managers (PBMs) began sending direct text alerts to patients when a drug they’re taking is recalled.Pilot programs show this cuts response time by 35%. Soon, you might get a text like: “Your valsartan (Lot L23AB78) is recalled. Call your pharmacy. Do not stop taking.”
But don’t wait for tech to save you. Even with better alerts, you still need to know what to do. The system works best when you’re informed - not just notified.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.