Constipation isn’t just an inconvenience-it’s a common, often misunderstood condition that affects one in three people who visit a doctor for digestive issues. If you’re going to the bathroom less than three times a week, struggling to pass hard stools, or feeling like you never fully empty your bowels, you’re not alone. But understanding what’s really going on-and how to fix it for good-is key to breaking the cycle of discomfort and dependency.
What Actually Causes Constipation?
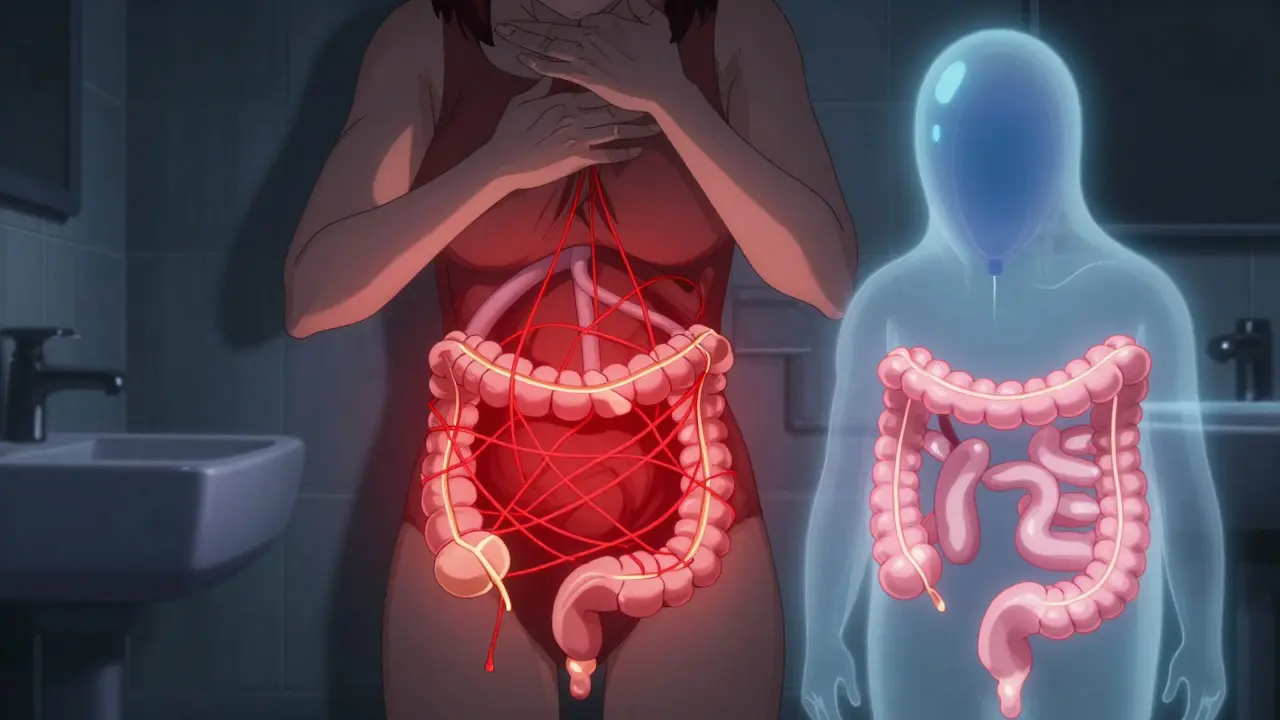
Constipation happens when stool moves too slowly through the colon, letting too much water get absorbed. The result? Hard, dry poop that’s tough to push out. But the reasons behind it aren’t always obvious.For many, it starts with lifestyle. The average American eats only about 15 grams of fiber a day-far below the recommended 25 to 30 grams. Add in not drinking enough water (less than 1.5 liters), sitting too much, or skipping meals, and you’ve set the stage for trouble. Even changes in routine-like traveling, switching jobs, or starting a new diet-can throw off your bowel habits.
But it’s not just about food and movement. Medications play a huge role. Opioids cause constipation in 40% to 95% of users. Calcium channel blockers like nifedipine and tricyclic antidepressants are common culprits too. Diabetes? Nearly 60% of people with the condition deal with constipation. Hypothyroidism, Parkinson’s, multiple sclerosis, and even past strokes can slow down your digestive system. These aren’t just side effects-they’re direct contributors.
Women are more likely to experience it, especially after age 60. And while it’s often dismissed as "just part of aging," it’s not normal. If you’ve noticed a change in your bowel habits lasting more than six weeks, especially with weight loss or blood in your stool, you need to get checked. These are alarm signs that could point to something more serious.
Types of Constipation: It’s Not All the Same
Not everyone with constipation has the same problem. Doctors break it down into four main types, and each needs a different approach.Normal transit constipation (the most common, affecting 60% of chronic cases) means your stool moves through your colon at a normal pace-but you still feel like you can’t go. You strain, feel incomplete, and pass hard stools. This is often tied to diet, stress, or ignoring the urge to go.
Slow transit constipation (15-30% of cases) means your colon is sluggish. Stool takes more than 72 hours to move through. It’s common in older adults and people with long-standing issues. You might go once every few days and feel bloated all the time.
Defecatory disorders affect 20-50% of chronic cases. This isn’t about speed-it’s about mechanics. Your pelvic floor muscles don’t relax properly when you try to poop. Instead of pushing stool out, they tighten up. You might feel like you’re pushing against a wall. A simple test-trying to expel a water-filled balloon in under a minute-can help diagnose this.
Refractory constipation affects 15-20% of people. These are the cases that don’t respond to standard treatments. You’ve tried fiber, water, laxatives-and nothing sticks. This often requires deeper investigation, including nerve testing or specialized medications.
Laxatives: What Works, What Doesn’t
Laxatives are everywhere-drugstores, online, even in your pantry. But not all of them are created equal. Some help. Some just mask the problem. A few can hurt you if used too long.Bulk-forming laxatives like psyllium (Metamucil) or methylcellulose (Citrucel) are safe and effective for many. They soak up water, swell up, and gently stimulate your colon. But they only work if you drink enough water-8 ounces per dose, minimum. Without it, they can actually make things worse by causing blockages.
Osmotic laxatives like polyethylene glycol (PEG 3350) are the first-line recommendation for most people. PEG draws water into the colon, softening stool without irritating the lining. It’s effective in 65-75% of cases, has minimal side effects, and is safe for long-term use. Lactulose and magnesium hydroxide work similarly but can cause gas or cramping.
Stimulant laxatives like senna or bisacodyl get things moving fast. They’re great for short-term relief-say, after surgery or during a flare. But using them for more than 2-3 weeks can damage your colon. Over time, your bowel stops responding naturally. This is called cathartic colon. Your colon becomes lazy. You need more and more to get the same result.
Stool softeners like docusate sodium? They’re popular, but don’t work well on their own. Studies show they’re only 10-15% better than a placebo. They’re fine as a helper, not a solution.
For stubborn cases, prescription options exist. Lubiprostone, linaclotide, and plecanatide work by increasing fluid secretion in the intestines. They’re effective for 40-60% of people with irritable bowel syndrome with constipation. But they’re expensive, and not for everyone.
Long-Term Management: Beyond the Pill
If you’re relying on laxatives year after year, you’re treating the symptom-not the cause. Real relief comes from rebuilding your system.Start with fiber-but go slow. Jumping from 15g to 30g overnight will make you bloated and gassy. Increase by 5g every 3-4 days. Focus on soluble fiber: oats, beans, apples, flaxseed. These are gentler and more effective than bran. Pair every 5g of fiber with an extra 250-500ml of water.
Hydration matters more than you think. Your colon pulls water from stool. If you’re dehydrated, it pulls harder. Aim for 1.5 to 2 liters of water daily. Coffee can help-it triggers the gastrocolic reflex, which kicks your bowels into gear after eating. But don’t use caffeine as a substitute for water.
Train your body to go. Set aside 10-15 minutes after breakfast to sit on the toilet. Don’t read, don’t scroll. Just sit. This trains your brain to associate that time with bowel movement. Elevate your feet on a stool so your hips are at a 35-degree angle. This straightens your rectum, making it easier to push. Studies show this reduces straining by 60%.
Biofeedback therapy is a game-changer for pelvic floor dysfunction. It uses sensors to show you how your muscles are working-and teaches you to relax them. After 6-8 weekly sessions, 70-80% of people see major improvement. It’s not magic. It’s retraining.
Medication should be a tool, not a crutch. Start with PEG 3350. If that doesn’t work, add a stimulant for short bursts. Only move to prescription drugs if everything else fails. And never use stimulant laxatives for more than 3 months. The American Gastroenterological Association warns: prolonged use can lead to colonic inertia, where your colon stops moving on its own.
When to See a Doctor
You don’t need to suffer in silence. But you also don’t need to assume every case is "just constipation."See a doctor if:
- You’ve lost weight without trying
- You notice blood in your stool
- Your bowel habits changed for more than 6 weeks
- You have a family history of colon cancer
- You’re taking medications and constipation started after
- You’ve tried diet, water, and laxatives for 3 months with no improvement
These aren’t "wait and see" situations. They’re red flags that could mean thyroid trouble, nerve damage, or even a tumor.
Real Stories, Real Results
One woman, 52, had been constipated for 15 years. She tried everything: prune juice, enemas, stimulant laxatives. Nothing lasted. She started with 25g of psyllium husk daily, drank 2 liters of water, drank coffee every morning, and sat on a footstool for 10 minutes after breakfast. Within 8 weeks, she was going regularly-no meds needed.Another man, 68, with Parkinson’s, struggled for years. His doctor recommended biofeedback. After 7 sessions, he went from once every 4 days to daily. He stopped using laxatives entirely.
These aren’t outliers. They’re examples of what happens when you stop treating the symptom and start fixing the system.
The Bigger Picture
Constipation costs the U.S. over $1.7 billion a year in medical care. It’s one of the most common reasons people miss work. And yet, most doctors spend less than 5 minutes talking about it. Patients often leave with a prescription and no real plan.But change is coming. New research is linking constipation to gut bacteria-like a drop in Bacteroides uniformis in 68% of patients. AI tools are now being tested to analyze how people strain during bowel movements using smartphone cameras. And new drugs like tenapanor are offering hope for those who haven’t responded to anything else.
The message is clear: constipation is treatable. But it takes patience, consistency, and the right approach. No pill alone will fix it. You need to change how you eat, drink, move, and even sit. The good news? Once you get it right, you won’t need to rely on laxatives anymore. Your body will start working the way it was meant to.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.