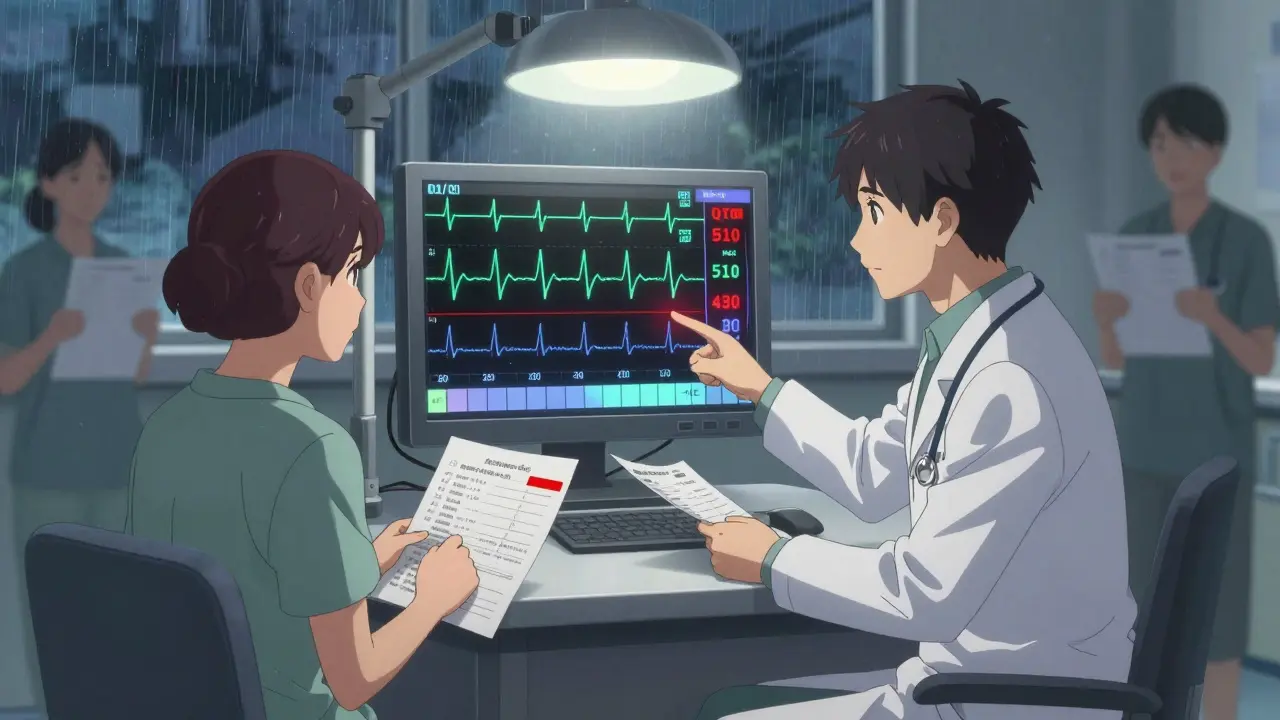
Methadone QT Prolongation Risk Calculator
Calculate your corrected QT interval (QTc) and assess risk of dangerous heart rhythms when taking methadone with other medications.
Enter Your Data
Results
When someone is on methadone for opioid dependence or chronic pain, their doctor usually checks for breathing issues, sedation, or liver function. But one of the most dangerous risks-methadone QT prolongation-often slips through the cracks. It doesn’t cause obvious symptoms until it’s too late. And when methadone is mixed with other common medications, that risk doesn’t just add up-it multiplies.
Why Methadone Is Different
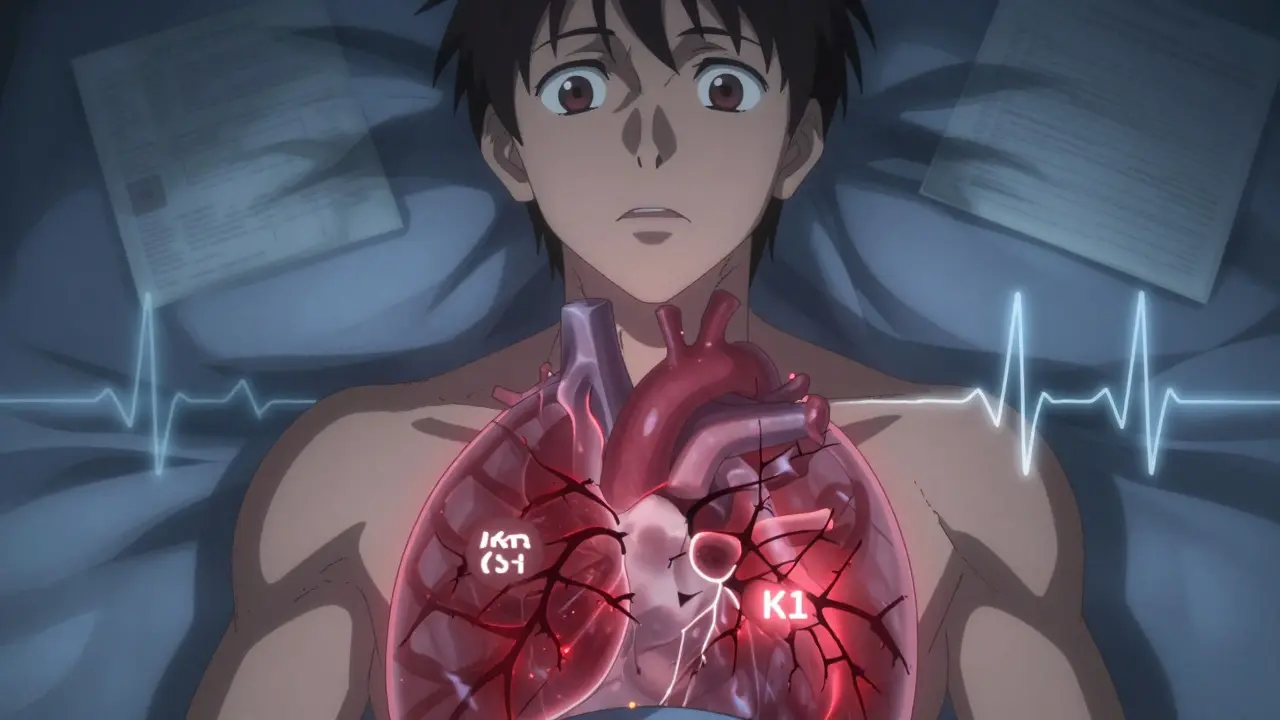
Methadone isn’t just another opioid. While drugs like buprenorphine barely touch the heart’s electrical system, methadone blocks two key potassium channels in heart cells: IKr and IK1. Most QT-prolonging drugs only block IKr. Methadone blocks both. That’s why it’s far more likely to trigger a life-threatening heart rhythm called torsades de pointes (TdP), even at doses that seem moderate.Think of it like a dam with two weak spots. One leak might be manageable. Two? The whole structure fails. That’s what happens in the heart. Methadone slows down the final phase of heart cell recovery, making the electrical signal uneven across the muscle. This creates the perfect setup for dangerous arrhythmias.
Studies show that after just 16 weeks of methadone therapy, nearly 70% of men and over 70% of women have a QTc interval above 450 milliseconds-the threshold where monitoring becomes critical. And in 1 in 10 patients, it climbs past 500 ms, a level linked to sudden cardiac death.
The Perfect Storm: When Drugs Combine
Methadone’s danger skyrockets when it’s paired with other QT-prolonging medications. This isn’t theoretical. Real cases have ended in death.Take antibiotics like erythromycin or clarithromycin. They’re common for sinus infections or bronchitis. Fluoroquinolones like moxifloxacin are used for pneumonia. Both prolong QT. When taken with methadone, they don’t just add to the risk-they push the heart into a dangerous zone faster than either drug could alone.
Antidepressants like citalopram or venlafaxine? Same story. Even antipsychotics like haloperidol, used for schizophrenia or severe anxiety, can be deadly in combination. And it’s not just prescription drugs. Cocaine, though short-acting, has been tied to TdP in methadone patients. One case report described a patient who developed persistent QT prolongation after using cocaine with methadone-even though the cocaine was long gone from their system.
Then there’s HIV treatment. Ritonavir, a common booster in antiretroviral regimens, does two bad things at once: it blocks the liver enzyme that breaks down methadone, causing methadone levels to spike, and it also prolongs QT. This double hit is why HIV-positive patients on methadone need especially close monitoring.
Who’s at Highest Risk?
Not everyone on methadone will have problems. But some people are walking into a minefield without knowing it.- Women (QTc thresholds are lower for women: 450 ms vs. 430 ms for men)
- People over 65
- Those with heart failure, prior heart attack, or structural heart disease
- Patients with low potassium or magnesium (common in people with poor nutrition or vomiting/diarrhea)
- Anyone taking two or more QT-prolonging drugs
- Those on methadone doses above 100 mg/day
Even if someone has none of these risk factors, methadone alone can still push QTc past 500 ms in 1 in 10 people. That’s why baseline testing isn’t optional-it’s essential.
What Doctors Should Do
Before starting methadone, every patient needs a baseline ECG. Not just any ECG-this one must be read by someone who knows how to measure QTc correctly. Many automated reports get it wrong, especially in people with wide QRS complexes or low voltage.After starting, repeat the ECG at 2 weeks, 4 weeks, and then every 3-6 months if stable. If the QTc goes above 450 ms in men or 470 ms in women, it’s time to reassess. If it hits 500 ms or increases by more than 60 ms from baseline, the risk of sudden death rises sharply.
There are three clear paths forward:
- Reduce the dose. One New Zealand patient had recurrent TdP at 120 mg/day. When the dose was cut to 60 mg/day, the QTc returned to normal.
- Switch to buprenorphine. Buprenorphine has 100 times less hERG blockade than methadone. For many patients, it’s just as effective for cravings and withdrawal-with far less cardiac risk.
- Correct electrolytes. Low potassium or magnesium makes QT prolongation worse. Simple blood tests and supplements can help.
Never just keep dosing up if QTc is rising. That’s how deaths happen.
What Patients Should Know
If you’re on methadone, you need to be your own advocate.- Ask your prescriber: “Has my QT interval been checked?” If they say no, insist on an ECG.
- Keep a list of every medication you take-prescription, over-the-counter, supplements, even herbal teas. Many people don’t realize that St. John’s Wort or certain cough syrups can prolong QT.
- If you feel dizzy, faint, or notice your heart racing or skipping beats, don’t wait. Go to the ER. These could be signs of TdP.
- Don’t stop methadone cold turkey. Withdrawal is dangerous. Talk to your doctor first.
The goal isn’t to scare you off methadone. It’s to make sure you’re safe while using it. Methadone saves lives. It reduces overdose deaths, cuts crime, and helps people rebuild. But those benefits vanish if the heart stops.
The Bigger Picture
Research from 2022 revealed something new: methadone doesn’t just block potassium channels-it may also reduce how many of those channels are even available in heart cells. That’s a deeper, longer-term effect, similar to how some cancer drugs damage the heart over time. This could explain why QT prolongation gets worse over months, even if the dose stays the same.Doctors are starting to look at new tools, like the Tpeak-Tend interval and U-wave analysis, to spot early signs of repolarization instability. These aren’t routine yet, but they’re coming.
For now, the message is simple: methadone is powerful. It works. But it’s not harmless. When paired with other drugs that affect the heart’s rhythm, the risk isn’t just higher-it’s predictable. And that means it’s preventable.
If you’re on methadone, get your ECG. Know your meds. Speak up. Your heart is worth it.

I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.