When you twist your ankle, slam your finger in the door, or wake up with a stiff lower back, you’re not just feeling pain-you’re experiencing nociceptive pain. This is the body’s most basic alarm system: tissue gets damaged, nerves scream, and your brain says, “Stop doing that!” It’s the reason you pull your hand away from a hot stove before you even think about it. Unlike nerve damage pain or mysterious chronic pain, nociceptive pain has a clear source: injured tissue. And knowing that changes everything about how you treat it.
What Exactly Is Nociceptive Pain?
Nociceptive pain isn’t just any ache. It’s pain caused by actual physical damage to skin, muscles, tendons, bones, or organs. The International Association for the Study of Pain defines it clearly: pain from real or threatened harm to non-nerve tissue. Think sprains, cuts, burns, arthritis flare-ups, or even a kidney stone. Your body has specialized nerve endings-called nociceptors-that detect bad stuff like extreme heat, pressure, or chemical changes from inflammation. When these fire off, you feel pain.
There are three main types:
- Superficial somatic: Sharp, pinpoint pain from skin injuries-like a paper cut or sunburn. These travel fast on Aδ fibers.
- Deep somatic: Dull, aching, hard-to-pinpoint pain from muscles, tendons, or bones. Think a strained back or broken rib. These use slower C fibers.
- Visceral: Deep, crampy, or pressure-like pain from inside organs-like gallstones or appendicitis. These are often vague and referred to other areas.
Here’s the key: nociceptive pain usually gets better as the tissue heals. That’s why a sprained ankle improves over days, not weeks. It’s not broken wiring like neuropathic pain-it’s a broken toe that needs time and the right treatment.
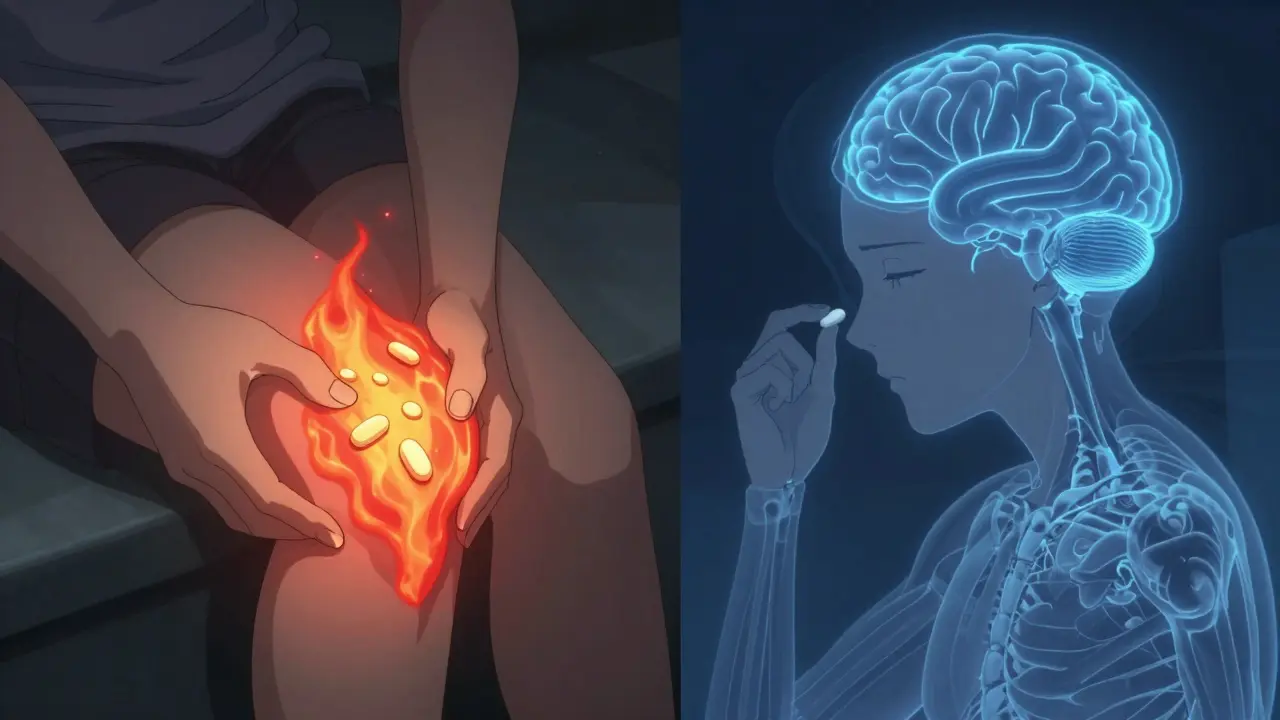
NSAIDs vs. Acetaminophen: The Real Difference
When you reach for pain relief, you’re probably choosing between ibuprofen (Advil, Motrin) or acetaminophen (Tylenol). They both reduce pain, but they work in completely different ways-and that matters a lot.
NSAIDs (non-steroidal anti-inflammatory drugs) target the source. They block enzymes called COX-1 and COX-2, which your body makes when tissue is injured. These enzymes trigger inflammation, swelling, and pain signals. By stopping them, NSAIDs reduce both the swelling and the pain. That’s why they’re so effective for sprains, arthritis, or post-surgery pain-where inflammation is the main problem.
Acetaminophen doesn’t touch inflammation at all. It works mostly in the brain and spinal cord, possibly by affecting serotonin pathways or a variant of the COX enzyme called COX-3. It dulls pain signals, but it doesn’t reduce swelling, redness, or heat. That’s why it’s fine for a headache or mild muscle ache, but won’t help much when your knee is swollen and hot.
Numbers don’t lie. A 2023 Cochrane Review of over 7,800 patients found that 49% of people got at least 50% pain relief from 400mg of ibuprofen after an acute injury. With placebo? Only 32%. Acetaminophen at 1,000mg? Just 39% relief for low back pain-significantly less than ibuprofen’s 48%.
When to Use NSAIDs (And When to Avoid Them)
NSAIDs are your go-to when there’s visible inflammation: swelling, warmth, redness, or stiffness. That means:
- Acute sprains or strains (ankle, wrist, hamstring)
- Arthritis flare-ups (knee, hip, hand)
- Post-surgical pain with swelling
- Tendonitis or bursitis
For best results, take ibuprofen 400-600mg every 6-8 hours within the first 2 hours of injury. Delaying reduces the anti-inflammatory effect. Studies show this can speed recovery by 2-3 days.
But NSAIDs aren’t risk-free. Long-term use increases your chance of stomach ulcers by 1-2% per year. High doses of diclofenac can double your risk of heart attack. That’s why the FDA requires black box warnings on all NSAID labels.
If you’re at risk for stomach issues-older adults, people on blood thinners, or those with a history of ulcers-talk to your doctor about combining NSAIDs with a proton pump inhibitor (like omeprazole). One study showed this cuts ulcer risk by 74%.
When Acetaminophen Makes Sense
Acetaminophen shines where there’s no swelling. Think:
- Tension headaches
- Mild back pain without inflammation
- Fever or post-viral aches
- Pain in people who can’t take NSAIDs
It’s the top choice for kids and older adults because it’s gentler on the stomach and kidneys. The American Headache Society recommends it as first-line for tension headaches-Level A evidence. And on Drugs.com, 74% of users reported high satisfaction for headaches, mostly because it doesn’t upset their stomach.
But here’s the catch: acetaminophen has one dangerous flaw-liver damage. The max safe daily dose is 4,000mg, but many people unknowingly overdose by taking multiple products that contain it (cold meds, sleep aids, combo pain relievers). As little as 150-200mg per kg of body weight can be fatal. The FDA tightened warnings in 2011 and now recommends no more than 3,000mg/day if you have liver issues or drink alcohol regularly.
What Do Real People Say?
On Reddit’s r/PainMedicine, 68% of 312 users said they prefer NSAIDs for acute injuries. One physical therapist wrote: “I tell patients to take 600mg ibuprofen three times a day for a sprained ankle. It reduces swelling and gets them walking faster.”
Meanwhile, acetaminophen fans on Drugs.com praise its safety. “No stomach burning. I can take it every day for my chronic back pain,” wrote one user. But others say: “It just doesn’t touch my knee pain. I need something stronger.”
Here’s the twist: 61% of chronic pain patients in a Mayo Clinic survey use both together. Combining 650mg acetaminophen with 400mg ibuprofen gave 32% better pain control than either alone. That’s not magic-it’s physics. One drug hits the brain, the other hits the inflammation. Together, they cover more ground.
What’s New in Pain Relief?
Science is catching up. Topical NSAID gels (like diclofenac) are now popular because they deliver pain relief with only 30% of the systemic exposure of pills-meaning fewer stomach or heart risks. Vimovo, a combo pill of naproxen and esomeprazole, cuts stomach ulcers by over half.
For acetaminophen, the FDA approved Qdolo in 2022-a mix of tramadol and acetaminophen-for moderate to severe pain. And researchers are testing drugs that target specific pain receptors in organs, like Eli Lilly’s LOXO-435, which is in trials for irritable bowel syndrome pain.
Market trends show NSAIDs still dominate acute care-89% of athletic trainers use them. But acetaminophen leads in pediatrics (92% of pediatricians) and geriatrics (68% of geriatricians) because of safety.
How to Choose the Right One
Here’s a simple decision tree:
- Is there swelling, redness, or warmth? → Go with NSAID (ibuprofen or naproxen).
- Is it a dull ache with no swelling? → Acetaminophen is fine.
- Do you have stomach issues, high blood pressure, or kidney disease? → Skip NSAIDs. Use acetaminophen-but stay under 3,000mg/day.
- Do you drink alcohol regularly? → Avoid acetaminophen. Use NSAIDs with caution and only short-term.
- Is the pain moderate to severe and not improving? → Talk to your doctor. You might need more than OTC meds.
Don’t assume “natural” or “gentler” means better. Acetaminophen isn’t safer for your liver just because it’s in every medicine cabinet. NSAIDs aren’t dangerous just because they’re strong. They’re tools. Use the right one for the job.
Final Takeaway
Nociceptive pain is your body’s way of saying, “Something’s broken here.” NSAIDs fix the broken part by reducing inflammation. Acetaminophen just mutes the alarm. If your tissue is inflamed, NSAIDs win. If it’s just sore, acetaminophen works-and it’s gentler. But never mix them without knowing the dose. And never ignore pain that doesn’t improve in a few days. Sometimes, the real problem isn’t the painkiller-it’s the injury underneath.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.