Every year, tens of thousands of patients in the U.S. are harmed or killed by medication errors - many of them preventable. These aren’t just mistakes made by tired pharmacists. They’re often the result of broken workflows, handwritten prescriptions, missed drug interactions, or mislabeled vials. The solution isn’t more caffeine or longer shifts. It’s pharmacy workflow and error prevention systems - technology designed to catch mistakes before they reach the patient.
How Medication Errors Happen in Pharmacies
Pharmacists aren’t careless. They’re overloaded. A single community pharmacy might fill 300-500 prescriptions a day. Each one requires checking the patient’s name, drug, dose, route, frequency, allergies, and interactions. One slip-up - like confusing levothyroxine with levodopa - can be deadly. Manual processes are the biggest risk. A 2023 study in the Journal of the American Pharmacists Association found that 68% of dispensing errors occurred during manual entry or verification steps. That’s why pharmacies are turning to automation.What Pharmacy Workflow Systems Actually Do
Modern pharmacy workflow systems aren’t just fancy scanners. They’re integrated platforms that guide every step of the medication journey - from prescription receipt to patient handoff. Here’s how they work in practice:- When a prescription arrives electronically, the system auto-checks the patient’s profile for allergies and drug interactions.
- It flags duplicate therapies or dosing errors before a pharmacist even sees it.
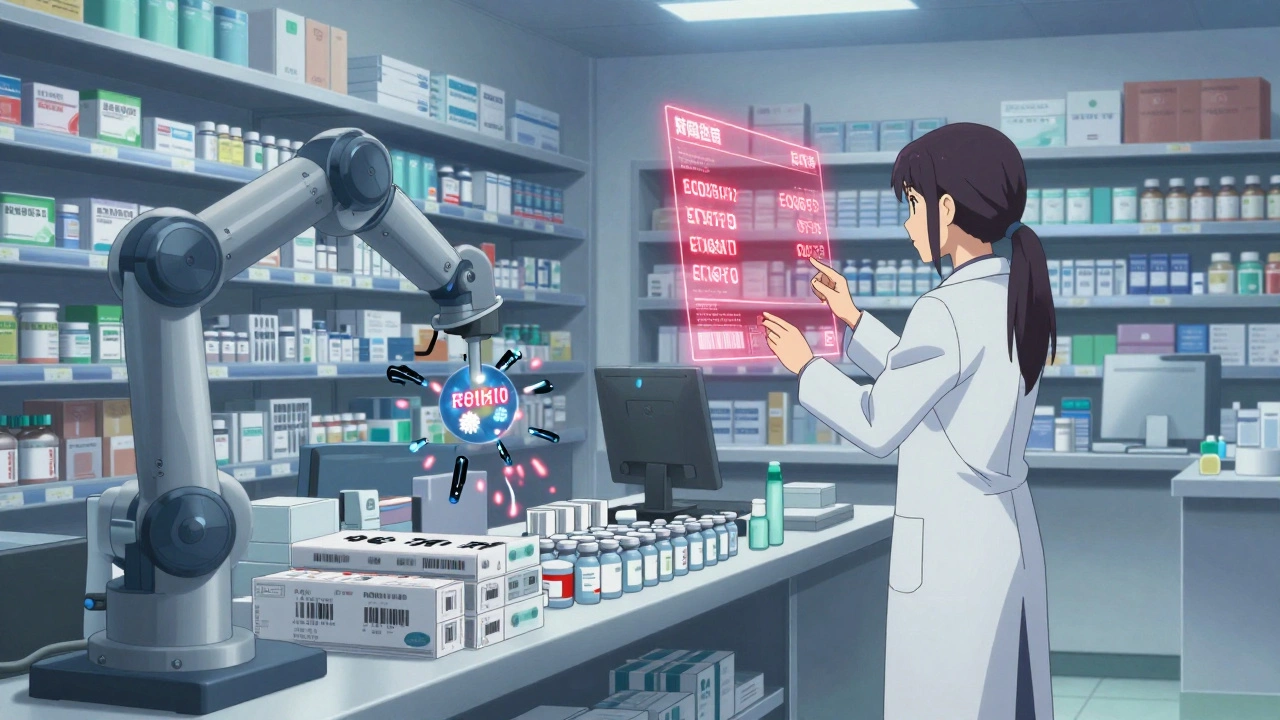
- Robotic arms pick the right bottle from inventory based on barcode matching.
- Each vial is scanned twice: once when taken from shelf, again when packaged.
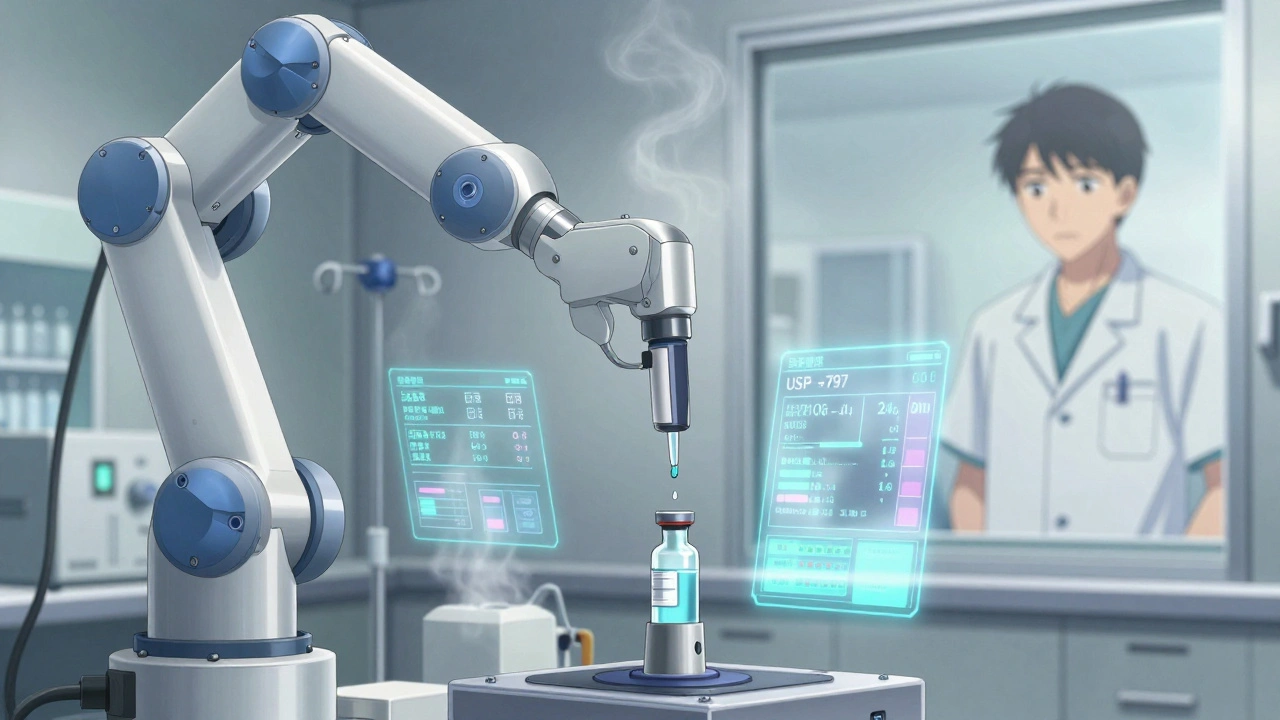
- IV compounding robots measure exact volumes of drugs and diluents - down to the microliter - with built-in weight sensors.
- All steps are logged in real time and synced with the hospital’s electronic health record (EHR).
This isn’t science fiction. Systems like BD Pyxis™ and Wolters Kluwer’s Simplifi+ IV are already in use at over 70% of U.S. hospitals. They don’t replace pharmacists - they free them from repetitive tasks so they can focus on complex cases and patient counseling.
Key Components of an Effective System
Not all pharmacy workflow tools are the same. The most effective ones include these five core pieces:- Barcode Verification - Every medication bottle and patient wristband must be scanned. If the barcode doesn’t match, the system stops the process.
- Drug Interaction Alerts - Real-time checks against databases like Micromedex or Lexicomp. If a patient is on warfarin and the script calls for amiodarone, the system screams.
- Inventory Tracking - Alerts when stock is low or drugs are expiring. No more handing out expired insulin.
- HL7 Integration - Two-way communication with EHRs. The system pulls lab results, diagnosis codes, and current meds so the pharmacist has full context.
- Workflow Automation - Tasks are assigned, tracked, and escalated automatically. A refill request goes to the tech, then the pharmacist, then the pickup queue - no paper trails.
These systems don’t just reduce errors. They cut dispensing time by up to 40%. One 2024 audit at a Midwest hospital showed that after implementing a full workflow system, average prescription fill time dropped from 22 minutes to 13 minutes - and error rates fell by 89%.
Types of Systems Used Today
There’s no one-size-fits-all solution. Pharmacies choose based on their needs:| System Type | Best For | Key Features | Typical Cost (Annual) |
|---|---|---|---|
| Enterprise Pharmacy Systems (Epic, Cerner) | Large hospitals, integrated health networks | Full EHR integration, multi-site inventory, compliance reporting | $150,000-$250,000 |
| IV Compounding Systems (Simplifi+, Pyxis) | Hospital IV labs, infusion centers | Robotic compounding, sterile environment monitoring, USP <797> compliance | $80,000-$180,000 |
| Cloud-Based Workflow Tools (Cflow, Kissflow) | Independent pharmacies, small clinics | Customizable templates, mobile access, reporting dashboards | $20,000-$60,000 |
| Central Fill Systems | Health systems managing prescriptions for multiple locations | Batch processing, automated labeling, shipping integration | $100,000-$200,000 |
Smaller pharmacies don’t need a $200,000 system. A cloud-based tool like Cflow can cut errors by 60% with a fraction of the cost. The key is matching the system to your workflow - not forcing your workflow to fit the system.
Why Technology Alone Isn’t Enough
Installing a robot doesn’t fix a broken process. Many pharmacies fail because they treat automation like a magic button. The American Society of Health-System Pharmacists (ASHP) found that pharmacies with the best outcomes didn’t just buy software - they redesigned their entire workflow around it.Successful implementations include:
- Training every staff member - techs, pharmacists, and even clerks - on how the system works.
- Running mock error drills to test the system’s alerts.
- Creating a “change champion” on each shift to answer questions and troubleshoot.
- Measuring outcomes: tracking how many errors were caught, how long prescriptions took, and whether patient complaints dropped.
One 340B hospital in Ohio spent six months training staff before turning on the new system. They didn’t rush. The result? A 92% drop in documentation errors and zero medication-related adverse events in the first year.
Real-World Impact: Numbers That Matter
The data doesn’t lie:- Systems with barcode scanning and robotic verification detect 14 times more errors than manual processes.
- Hospitals using automated IV compounding saw a 75% reduction in contamination-related failures.
- Community pharmacies using workflow software reduced dispensing errors by 65-80% within 12 months.
- Pharmacies with real-time EHR integration cut medication reconciliation errors by 85%.
These aren’t theoretical gains. They’re lives saved. A 2025 analysis from the CDC found that if every U.S. hospital adopted automated pharmacy systems, preventable medication deaths could drop by more than 20,000 per year.
Challenges and Pitfalls
No system is perfect. Common problems include:- High upfront cost - Smaller pharmacies struggle to justify $50K+ investments.
- Staff resistance - Some pharmacists fear being replaced. The truth? They’re freed from grunt work to do higher-value tasks.
- Integration headaches - If the system doesn’t talk to your EHR or billing software, it becomes a siloed tool.
- Over-reliance - Technicians might skip double-checks because “the system said it’s fine.” Human oversight is still required.
The biggest mistake? Buying a system and calling it done. Implementation takes 3-6 months. You need ongoing training, feedback loops, and regular audits.
What’s Next? AI and Predictive Workflow
The next wave of pharmacy systems isn’t just reactive - it’s predictive. New tools use AI to:- Anticipate which drugs will run out before the next delivery.
- Flag patients at high risk for adverse reactions based on history and genetics.
- Automatically suggest safer alternatives when a high-risk drug is prescribed.
- Adjust staffing levels based on daily prescription volume trends.
One pilot program in California used AI to predict insulin shortages 11 days in advance - allowing the pharmacy to reorder before patients were left without medication. That’s the future: not just preventing errors, but preventing crises before they start.
Regulations and Compliance
You can’t just install any software. Pharmacy systems must comply with:- USP <797> - For sterile compounding environments (clean rooms, air quality, gowning protocols).
- USP <800> - For handling hazardous drugs (chemotherapy, antivirals).
- HIPAA - All patient data must be encrypted and access-controlled.
- DEA regulations - For controlled substances, systems must track every pill.
Non-compliance isn’t just risky - it’s illegal. Systems that don’t meet these standards are being pulled from hospitals. Always ask vendors: “Can you show me your USP <797> and HIPAA compliance certification?”
Do pharmacy workflow systems really reduce errors?
Yes. Studies show systems with barcode scanning and automation detect 14 times more errors than manual processes. Hospitals using these systems report 75-90% drops in dispensing mistakes. The key is combining technology with proper training - not just installing software.
How much do pharmacy workflow systems cost?
Costs vary widely. Enterprise hospital systems range from $150,000 to $250,000 per year. Smaller pharmacies can use cloud-based tools like Cflow or Kissflow for $20,000-$60,000 annually. IV compounding robots cost $80,000-$180,000. Most vendors offer tiered pricing based on pharmacy size and features.
Can small pharmacies afford these systems?
Absolutely. You don’t need a $200,000 robot. Cloud-based workflow tools like Cflow or Kissflow offer error-checking, inventory alerts, and prescription tracking for under $50,000 a year. Many small pharmacies cut errors by 60% with these affordable options.
Do these systems replace pharmacists?
No. They free pharmacists from repetitive tasks like counting pills or checking for obvious interactions. That lets them focus on complex cases, patient counseling, and clinical decision-making - which is exactly what they were trained to do.
How long does it take to implement a pharmacy workflow system?
Most implementations take 3 to 6 months. This includes staff training, system integration, testing, and workflow redesign. Rushing the process leads to errors and resistance. Successful pharmacies treat this like a cultural shift - not just a tech upgrade.
What’s the biggest mistake pharmacies make when adopting these systems?
Believing that buying the software is the end goal. The real work starts after installation: training staff, adjusting workflows, measuring outcomes, and fixing gaps. The most successful pharmacies treat automation as a continuous improvement project - not a one-time purchase.
Next Steps for Pharmacies
If you’re considering a workflow system, start here:- Map your current workflow. Where do errors happen most? Is it during intake? Verification? Labeling?
- Identify your top 3 pain points. Is it speed? Compliance? Staff burnout?
- Try a demo. Ask vendors to simulate your actual prescription volume.
- Ask for references. Talk to other pharmacies using the same system.
- Plan for training. Budget at least 4 weeks of staff time for learning and practice.
Medication errors aren’t inevitable. They’re a sign of a broken system. The right workflow technology, paired with smart people and good processes, can fix that. The goal isn’t just to avoid mistakes - it’s to build a pharmacy where patients can trust every pill they take.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.