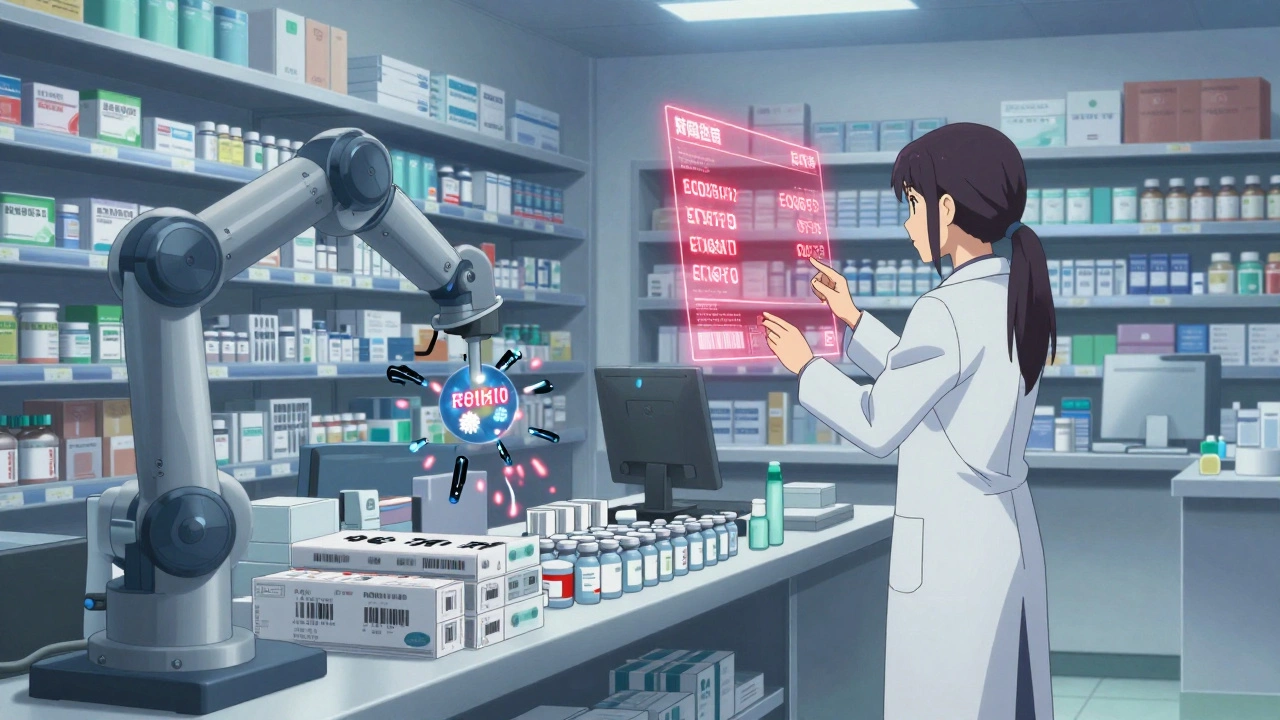
Pharmacy workflow and error prevention systems use automation, barcode scanning, and AI to cut medication errors by up to 90%. Learn how these tools work, which ones are best for your setting, and why simply buying software isn't enough.
When you take a pill, you expect it to help—not hurt. But medication errors, mistakes in how drugs are prescribed, dispensed, or taken that lead to harm. Also known as drug errors, they’re one of the most common causes of preventable injury in healthcare. These aren’t just rare accidents. They happen in hospitals, pharmacies, and homes—and often because of tiny oversights: a misread prescription, a wrong dose, or mixing pills that shouldn’t be taken together.
Dosing mistakes, incorrect amounts of medicine given or taken. Also known as medication overdoses or underdoses, it are especially dangerous for kids and older adults. Using a kitchen spoon instead of a proper syringe to give a baby acetaminophen? That’s a classic error. Or taking two painkillers that both contain acetaminophen without realizing it? That’s how liver damage starts. Even adults make these mistakes—like confusing similar-looking pills or forgetting they’re on a blood thinner and then taking an herb like Dong Quai that boosts bleeding risk. These aren’t just "oops" moments. They’re preventable.
Medication interactions, when two or more drugs, supplements, or even foods change how a medicine works in your body. Also known as drug interactions, it are silent killers. Caffeine can make warfarin less effective. Heatwaves can turn a normal dose of a painkiller into an overdose. Antibiotics like clindamycin can trigger life-threatening diarrhea. These aren’t theoretical risks—they show up in real cases every day. And they’re not always obvious. That’s why tracking your meds with a simple calendar or asking your pharmacist to check your full list matters more than you think.
Some errors come from the system—like combo generics that cost three times more than buying the same pills separately. Others come from confusion—like thinking "generic" means "less effective," when the real issue is whether your body absorbs it the same way. The 80-125% rule for generics isn’t about ingredients—it’s about how your body uses them. And if you’re on a drug like lithium or warfarin, missing a single lab test can mean the difference between safety and crisis.
You don’t need to be a doctor to stop these errors. You just need to ask questions. What’s this pill for? What happens if I miss a dose? Can I take this with my coffee? Is this the right dose for my weight or age? Simple steps like using a pill organizer, keeping a written list of everything you take, and never guessing a dose can cut your risk dramatically. The posts below show you exactly how these mistakes happen—and how real people are avoiding them every day. From inhaler technique that keeps medicine in your lungs instead of your throat, to how to space probiotics with antibiotics to protect your gut, these aren’t theory lessons. They’re survival tips.
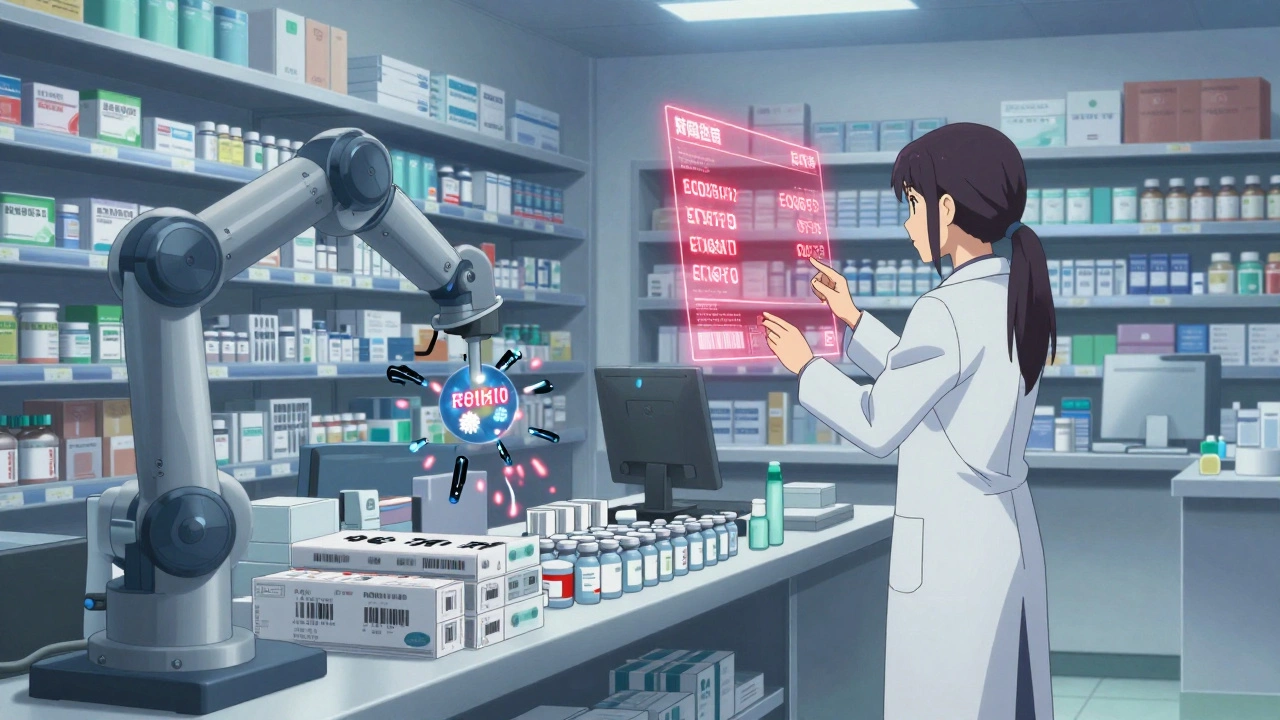
Pharmacy workflow and error prevention systems use automation, barcode scanning, and AI to cut medication errors by up to 90%. Learn how these tools work, which ones are best for your setting, and why simply buying software isn't enough.