Every time you pick up a prescription and see a lower price than expected, chances are you’re holding a drug approved through an ANDA. But what exactly is an ANDA, and why does it matter to you? It’s not just a bureaucratic term-it’s the reason generic drugs exist, and it’s one of the biggest reasons prescription costs in the U.S. have dropped so dramatically over the last 40 years.
What Is an ANDA?
An Abbreviated New Drug Application, or ANDA, is the official form drug companies submit to the U.S. Food and Drug Administration (FDA) to get approval to sell a generic version of a brand-name medicine. Unlike brand-name drugs, which need full clinical trials to prove they’re safe and effective, generic drugs don’t have to start from scratch. That’s what “abbreviated” means here-they skip the expensive and time-consuming human trials because they’re proving they work the same way as a drug that’s already been approved.
The ANDA pathway was created by the Hatch-Waxman Act in 1984. Before that, generic drugs faced huge legal and regulatory barriers. The law changed everything. It gave generic manufacturers a clear path to market while still protecting the patents of original drug makers. Today, more than 90% of all prescriptions filled in the U.S. are for generic drugs approved through ANDAs.
How Does an ANDA Work?
For a generic drug to get approved via ANDA, it must meet strict criteria. The FDA requires proof that the generic is:
- Identical in active ingredient
- The same strength and dosage form (pill, injection, cream, etc.)
- Given the same way (oral, topical, injected)
- Used for the same medical conditions
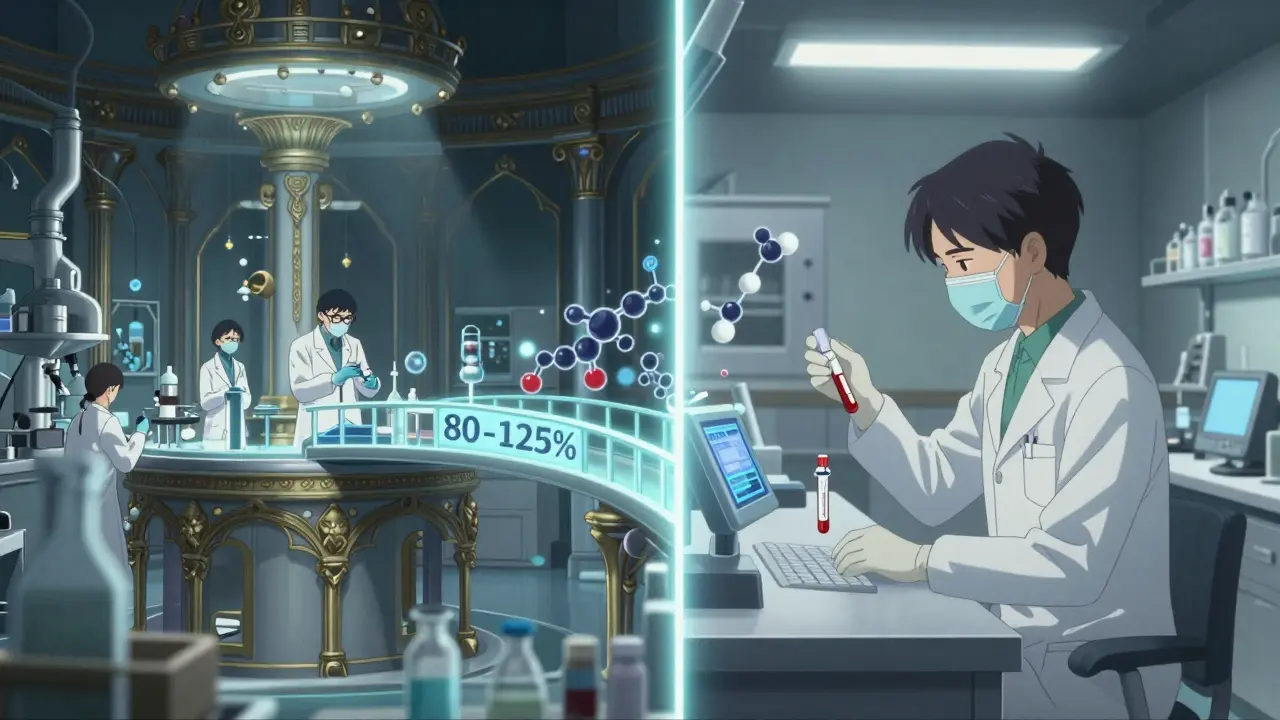
That’s the easy part. The real test is bioequivalence. This means the generic drug must enter your bloodstream at the same rate and in the same amount as the brand-name version. To prove this, manufacturers run small studies-usually with 24 to 36 healthy volunteers. They measure how quickly the drug is absorbed and how long it stays in the body. The results must fall within 80% to 125% of the brand-name drug’s performance for both key metrics: AUC (total exposure) and Cmax (peak concentration).
Think of it like this: if the brand-name drug gives you 100 units of medicine over 8 hours, the generic must deliver between 80 and 125 units over the same time. That’s not a wide range-it’s tight enough to ensure no noticeable difference in how the drug works.
What’s Not Allowed in an ANDA?
Not every drug can go generic. Complex drugs-like inhalers, injectables with special delivery systems, or topical creams that work on the skin’s surface-don’t always fit the standard ANDA model. Why? Because it’s hard to prove they behave the same way just by measuring blood levels. For example, a generic asthma inhaler might contain the same active ingredient, but if the propellant or nozzle design changes, the drug might not reach the lungs the same way. Those require special studies and are still being worked into the ANDA framework.
Also, you can’t submit an ANDA while the brand-name drug’s patent is still active. The Hatch-Waxman Act lets generic companies challenge those patents, but if they do, the FDA can delay approval for up to 30 months while legal battles play out. That’s why the first company to file an ANDA for a popular drug often gets 180 days of exclusive rights to sell it before others can join. That’s what led to a flood of generic versions of Humira (adalimumab) hitting the market in 2023.
ANDA vs. NDA: The Big Difference
Let’s compare the two paths:
| Feature | ANDA (Generic) | NDA (Brand-Name) |
|---|---|---|
| Time to approve | 10 months (standard) | 10-12 months |
| Cost to develop | $1-5 million | $2.6 billion |
| Clinical trials needed | No | Yes (Phase I-III) |
| Animal studies required | No | Yes |
| Approval success rate (first cycle) | 65% | 15-20% |
| Patent dependency | Must wait until patent expires or challenge it | Patent filed before approval |
The numbers speak for themselves. The NDA route is a decade-long, billion-dollar gamble. The ANDA route is a focused, science-based shortcut. And it’s why generic drugs cost 80-85% less than their brand-name equivalents within a year of launch.
Why Does the ANDA Pathway Matter?
It’s not just about saving money-it’s about access. In 2023, generic drugs saved the U.S. healthcare system $313 billion. That’s not a guess. That’s the official number from the Association for Accessible Medicines. Without ANDAs, millions of people wouldn’t be able to afford insulin, blood pressure pills, antidepressants, or cancer treatments.
And it’s not just patients who benefit. Insurance companies, Medicare, Medicaid-all of them rely on generics to keep costs down. Hospitals stock generics because they’re reliable and affordable. Pharmacists recommend them because they’re proven. And doctors prescribe them because they know the outcomes are the same.
The FDA tracks every approved ANDA with a unique six-digit number-like ANDA 214,455 for the generic version of Eliquis. Each one represents a drug that’s been reviewed, tested, and cleared. Over 11,000 ANDAs have been approved since 1984. That’s more than 11,000 chances for someone to get the medicine they need without going broke.
Challenges and Criticisms
It’s not perfect. The FDA’s own data shows that 32% of ANDA rejections come down to manufacturing issues-poor quality control, inconsistent production lines, or unapproved changes in the process. Another 27% are due to weak bioequivalence data. Many small manufacturers struggle with the complexity. One survey found that 68% of smaller companies got hit with a “complete response letter” from the FDA-meaning they had to resubmit with more data.
There’s also a growing concern about where these drugs are made. Over half of all generic drug ingredients come from India and China. A 2023 Health Affairs article warned that this concentration creates supply chain risks. If a single factory shuts down, it can cause nationwide shortages of critical drugs.
And while the FDA has made progress-reducing review times by 35% since 2018 thanks to the GDUFA program-there’s still a long way to go. The goal is to get 90% of ANDAs approved on the first try by 2027. Right now, it’s only 65%.

What’s Next for ANDAs?
The future is in complexity. More ANDAs are being filed for tricky drugs-like nasal sprays, transdermal patches, and long-acting injectables. The FDA has started releasing special guidance for these, and industry analysts expect complex generics to make up 25% of the market by 2028. That’s up from 15% today.
There’s also talk of expanding the ANDA model to include more biosimilars-drugs based on biological molecules like antibodies. But those follow a different rulebook under the BPCIA. ANDAs are still for small-molecule drugs, which make up the vast majority of prescriptions.
One thing’s certain: as long as people need affordable medicine, the ANDA pathway will stay vital. The Congressional Budget Office estimates that between 2024 and 2033, generic drugs will save the U.S. $1.7 trillion. That’s not just a number-it’s thousands of people who can keep taking their meds because they can afford them.
How to Find an ANDA-Approved Generic
If you’re curious whether your generic drug has been properly approved, check Drugs@FDA. Search for the brand name, then look under “Therapeutic Equivalence” for the “AB” rating. That means it’s approved as equivalent. If you see “BX,” it’s not rated equivalent-usually because it’s a complex product with unclear bioequivalence data.
Also, if your pharmacist switches your brand to a generic, ask if it’s an ANDA-approved version. Most are. But knowing the difference helps you understand why the price dropped-and why it’s still safe.
Is a generic drug the same as the brand-name version?
Yes, for all practical purposes. Generic drugs contain the same active ingredient, work the same way, and have the same risks and benefits as the brand-name version. The only differences are in inactive ingredients (like dyes or fillers), packaging, and price. The FDA requires proof of bioequivalence, meaning the drug performs identically in your body. Studies show 97% of generic drugs are therapeutically equivalent to their brand-name counterparts.
Why are generic drugs cheaper?
Generic drugs don’t have to repeat expensive clinical trials. The original drug maker already proved safety and effectiveness. Generic manufacturers only need to show their version is bioequivalent, which costs between $1 million and $5 million-far less than the $2.6 billion it takes to bring a new drug to market. Competition among multiple generic makers also drives prices down further.
Can I trust a generic drug?
Absolutely. The FDA inspects every manufacturing facility that produces generic drugs-same as brand-name ones. In fact, many brand-name companies also make their own generics. The FDA requires the same quality standards, and drugs are routinely tested after approval. If a generic fails, it’s pulled from the market. Millions of people use generics safely every day.
How long does it take to get an ANDA approved?
Under current rules, the FDA has 10 months to review a standard ANDA. But it often takes longer due to incomplete submissions or requests for more data. On average, companies wait 12-18 months from submission to approval. The first company to file an ANDA for a drug after patent expiry can get 180 days of exclusive marketing rights, which speeds up their return on investment.
What happens if my generic drug doesn’t work like the brand?
If you notice a difference in how you feel after switching to a generic, talk to your doctor or pharmacist. In rare cases, people may react differently to inactive ingredients-like dyes or fillers-or to a different release profile in extended-release versions. But true differences in effectiveness are extremely rare. The FDA requires strict bioequivalence standards. If a pattern emerges, the FDA investigates and may withdraw approval.
Are all generics made in the U.S.?
No. The majority of active pharmaceutical ingredients for generics come from India and China. Final manufacturing and packaging may happen in the U.S., Europe, or elsewhere. The FDA inspects all facilities, regardless of location. About 50% of generic drug manufacturing sites are overseas. While this keeps costs low, it also creates supply chain risks, especially during global disruptions.
Final Thoughts
The ANDA isn’t flashy. It doesn’t make headlines. But it’s one of the most powerful tools in modern medicine. It turns patents into competition, high prices into affordability, and inaccessible treatments into everyday pills. It’s the quiet engine behind the generic drug revolution-and it’s working.
Every time you choose a generic, you’re not just saving money. You’re supporting a system that keeps millions of people healthy without bankrupting them. That’s the real power of an ANDA.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.