When a patient walks in with shortness of breath, swollen ankles, or unexplained fatigue, the question isn’t just "Is this heart failure?" - it’s "Can I rule it out fast, safely, and without wasting time or money?" That’s where NT-proBNP blood testing comes in. It’s not just another lab order. It’s often the difference between a 3-day hospital stay and a quick discharge, between an unnecessary echocardiogram and a clear diagnosis.
Why NT-proBNP? The Science Behind the Test
NT-proBNP stands for N-terminal pro-B-type natriuretic peptide. It’s a protein fragment released by the heart when the ventricles are stretched - usually because they’re working too hard, often due to fluid overload or weakening muscle. Unlike BNP, which breaks down quickly in the blood, NT-proBNP is stable for hours. That means labs can process it even if the sample sits for a day. The Roche Elecsys® assay, used in over 70% of U.S. hospitals, can detect levels as low as 5 pg/mL with near-perfect precision.
The test isn’t perfect, but it’s powerful. At levels below 300 pg/mL, heart failure is ruled out with 98% accuracy. That’s not a guess - it’s backed by data from over 15,000 patients across multiple international studies. In emergency rooms, this single number can prevent hundreds of unnecessary imaging tests and admissions every year.
When to Order NT-proBNP: The Real-World Indications
Clinicians don’t order this test for everyone. It’s targeted. Here’s when it’s most useful:
- Acute dyspnea in the ER: If a patient comes in struggling to breathe, especially if they’re over 60 or have a history of heart disease, order NT-proBNP before imaging. Levels under 300 pg/mL mean heart failure is extremely unlikely - and you can look elsewhere.
- Unexplained fatigue or edema in older adults: Many seniors get tired or puffy legs. Is it heart failure, kidney issues, or just aging? NT-proBNP helps separate the causes. A level of 1,200 pg/mL in a 75-year-old with mild kidney disease might be normal for them - but 2,500 pg/mL? That’s a red flag.
- Monitoring known heart failure: If a patient is on diuretics or new heart meds, checking NT-proBNP every 3-6 months shows if treatment is working. A drop of 30% or more often means improved outcomes.
- Post-acute coronary syndrome: New guidelines from the 2024 ACC/AHA update now recommend testing after a heart attack. High NT-proBNP levels predict higher risk of death or hospitalization in the next year.
Don’t order it for routine checkups. Don’t test asymptomatic patients. Medicare started rejecting those in January 2025 - and for good reason. Studies show 18% of tests were ordered without clinical justification, driving up costs without improving care.
Age, Kidney Disease, and Obesity: The Three Big Confounders
NT-proBNP is simple - until it isn’t. Three factors change what "normal" means:
- Age: Levels rise naturally as you get older. For patients under 50, the cutoff is 450 pg/mL. Between 50-75, it’s 900 pg/mL. Over 75? 1,200 pg/mL. Ignore this, and you’ll overdiagnose heart failure in healthy seniors.
- Chronic kidney disease (CKD): The kidneys clear NT-proBNP. In stage 3-4 CKD, levels rise 28-40% even without heart failure. Use the adjusted cutoff: rule out heart failure at <1,200 pg/mL, not 300. Always check eGFR before interpreting.
- Obesity: Fat tissue suppresses NT-proBNP. For every 5-point increase in BMI, levels drop 25-30%. A 300 pg/mL reading in a patient with BMI 40 might actually mean significant heart strain. Don’t dismiss elevated levels in thin patients - but don’t overreact to normal levels in obese ones.
There’s no single number that fits everyone. That’s why the Heart Failure Society of America runs a free interpretation hotline. Clinicians call it over 1,200 times a month. It’s not a crutch - it’s a safety net.
NT-proBNP vs. BNP: Why NT-proBNP Won
There are two natriuretic peptide tests: BNP and NT-proBNP. So why does NT-proBNP dominate 68% of U.S. orders?
| Feature | NT-proBNP | BNP |
|---|---|---|
| Half-life in blood | 60-120 minutes | 20 minutes |
| Sample stability | 72 hours at 4°C | 4 hours at room temp |
| Diagnostic accuracy (AUC) | 0.91 | 0.88 |
| Renal clearance impact | High - requires adjustment | Lower |
| Obesity effect | 25-30% reduction per 5 BMI units | 15-20% reduction |
| Market share (U.S.) | 68% | 32% |
NT-proBNP wins because it’s more reliable. If a sample sits in the lab for hours? No problem. If a patient is obese? You know how to adjust. If you’re in a rural hospital without immediate access to testing? NT-proBNP still gives you usable results the next day.
What the Experts Say - And What They Warn Against
Dr. James Januzzi Jr. from Harvard calls NT-proBNP "the single most useful blood test in the evaluation of dyspnea." That’s not hype - it’s based on decades of outcome data. A 2023 Medscape survey found 89% of cardiologists consider it essential.
But Dr. Allan Jaffe from Mayo Clinic warns: "Never use it alone." I’ve seen cases where a 78-year-old with atrial fibrillation and stage 3 CKD had an NT-proBNP of 850 pg/mL. Was it heart failure? Or just aging, AFib, and kidney changes? Without echocardiography, clinical history, and physical exam, you can’t tell. The test is a gatekeeper - not a diagnostic oracle.
One cardiologist on Reddit shared how NT-proBNP saved her from ordering a $3,000 echo for an 82-year-old with COPD. The level was 120 pg/mL. She treated the lung infection instead. No hospital stay. No cost. No risk.
What’s New in 2025: Point-of-Care and Policy Changes
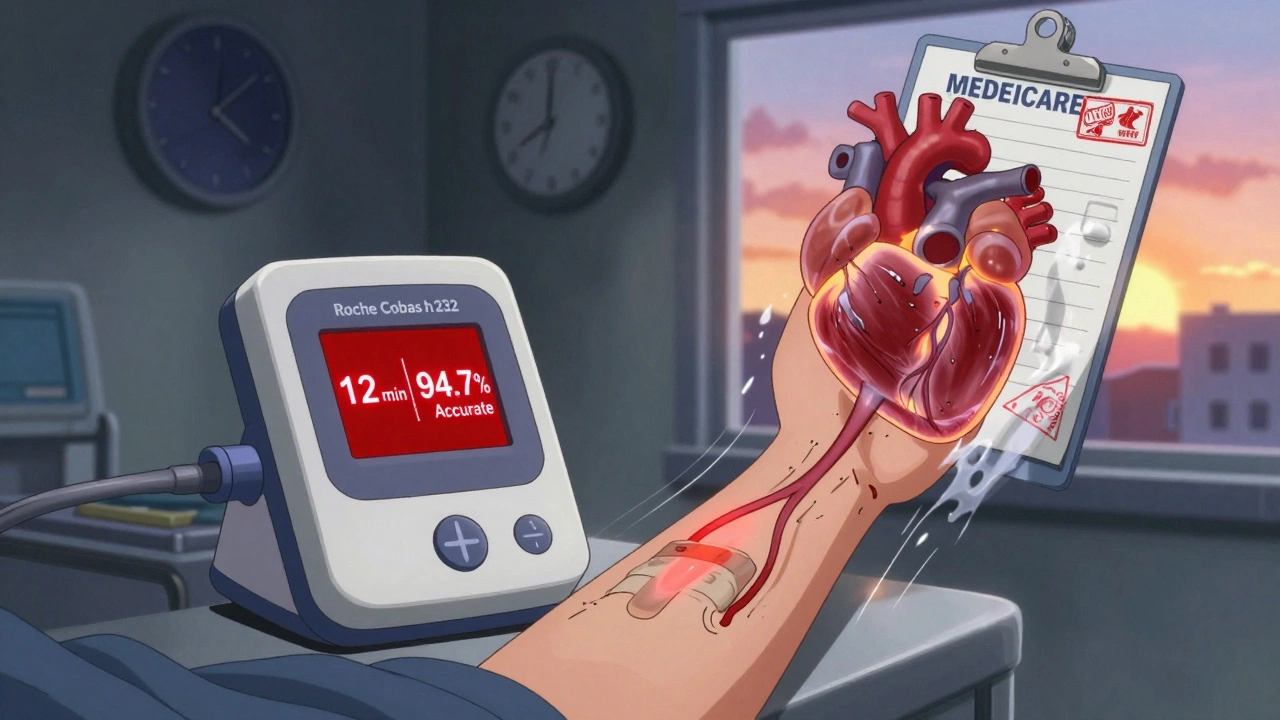
As of 2025, point-of-care NT-proBNP testing is now available in ERs and clinics. The Roche Cobas h 232 delivers results in 12 minutes - with 94.7% accuracy compared to lab results. This is changing how fast decisions get made. In trauma centers, they’re now testing within 15 minutes of arrival.
Medicare’s new prior authorization rules, starting January 2025, require documentation of symptoms before approving the test. That’s pushed hospitals to create standardized ordering protocols. Integrated health systems that did this saw inappropriate testing drop by 33%.
And it’s not slowing down. The global market for natriuretic peptide tests is now $1.2 billion and growing. Why? Because it works. It saves money. It saves time. And most importantly, it saves lives.
Practical Tips for Ordering and Interpreting
Here’s how to get it right:
- Order only when symptoms suggest heart failure: Dyspnea, fatigue, edema, orthopnea. Not for "routine screening."
- Check age and kidney function first: Adjust cutoffs. Don’t use 300 pg/mL for everyone.
- Don’t panic at moderately elevated levels: 500-1,000 pg/mL in an elderly patient with CKD might be their baseline. Look for trends.
- Use it to guide next steps: Low level? Rule out heart failure and investigate other causes. High level? Order echo, start diuretics, refer to cardiology.
- Re-test after treatment: A 30% drop in 4-6 weeks means therapy is working. No drop? Time to rethink the plan.
There’s no magic formula. But if you learn the cutoffs, understand the confounders, and use it with clinical judgment - NT-proBNP becomes your most reliable tool in the chest pain and dyspnea workup.
Is NT-proBNP testing covered by insurance?
Yes, Medicare and most private insurers cover NT-proBNP testing when ordered for symptomatic patients with suspected heart failure. Starting January 2025, prior authorization is required to prevent testing in asymptomatic individuals. Reimbursement is around $18.42 per test under Medicare’s 2025 fee schedule.
Can NT-proBNP be used to diagnose heart failure in obese patients?
Yes, but levels are typically 25-30% lower per 5-point increase in BMI. A "normal" result in an obese patient may still indicate underlying heart strain. Always interpret results in context with symptoms, physical exam, and echocardiography. Never rely solely on NT-proBNP to rule out heart failure in someone with high BMI and clear clinical signs.
How often should NT-proBNP be repeated in heart failure patients?
For newly diagnosed patients, repeat testing at 3-6 weeks after starting treatment to assess response. For stable patients on maintenance therapy, testing every 3-6 months is sufficient to monitor disease progression. Rising levels over time often signal worsening heart function before symptoms appear.
Does kidney disease affect NT-proBNP results?
Yes. NT-proBNP is cleared by the kidneys, so levels rise in chronic kidney disease even without heart failure. For patients with stage 3-5 CKD, use an adjusted rule-out cutoff of <1,200 pg/mL instead of 300 pg/mL. Always check eGFR and creatinine alongside the NT-proBNP result.
Can NT-proBNP predict future heart failure in people without symptoms?
Elevated NT-proBNP in asymptomatic individuals is associated with higher long-term risk of developing heart failure, especially in those with hypertension, diabetes, or atrial fibrillation. However, current guidelines do not recommend routine screening in healthy people. The test is best used for diagnosis and monitoring - not population screening.
What Comes Next?
NT-proBNP isn’t going away. Even as new biomarkers emerge - like galectin-3 or ST2 - none have matched its 28 years of outcome data. It’s the anchor. The standard. The test that tells you, with near certainty, whether the heart is failing - or if the problem lies somewhere else.
What’s changing is how we use it. Faster results. Better guidelines. Fewer unnecessary tests. More confidence. And for clinicians, that means less guesswork - and more time to treat the patient, not the number.

I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.