When your liver starts to scar, it’s not just a minor warning-it’s a major red flag. Cirrhosis isn’t a single disease. It’s the end result of years of damage, where healthy liver tissue gets slowly replaced by tough, fibrous scar tissue. This isn’t something that happens overnight. It creeps up silently, often without symptoms, until one day, your body can’t keep up anymore. By then, the damage is mostly permanent. But here’s the thing: if you catch it early, you can still stop it from getting worse. And if it’s too far gone, liver transplantation might be the only lifeline left.
What Exactly Is Cirrhosis?
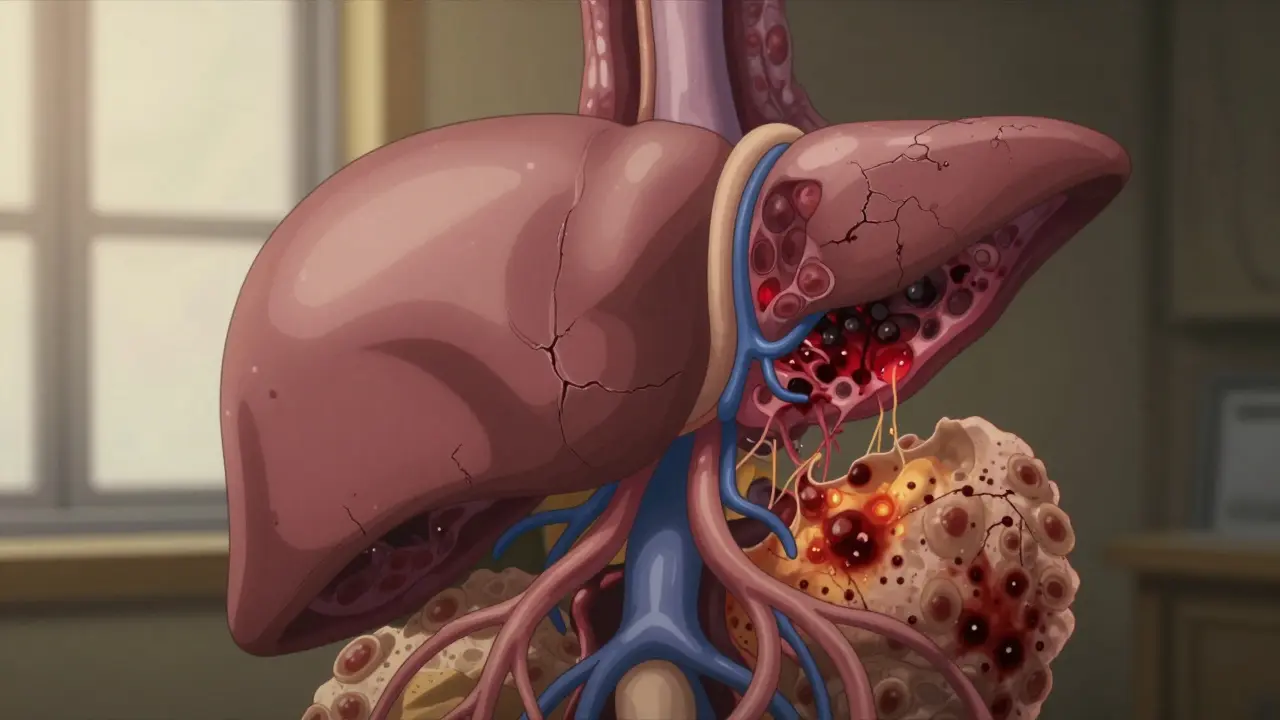
Cirrhosis means your liver has been damaged so badly that it can’t repair itself properly. Instead of healing, it builds scar tissue. This scar tissue doesn’t work like real liver tissue. It doesn’t filter toxins, make proteins, or help digest food. Over time, these scars pile up, twisting the liver’s structure into a lumpy, stiff mess. The liver is one of the few organs that can regenerate, but once cirrhosis sets in, that ability is overwhelmed.
The term comes from the Greek word kirrhos, meaning tawny yellow-the color a damaged liver often turns. But the color doesn’t matter as much as what’s happening inside. Healthy liver cells (hepatocytes) are replaced by fibrous bands that block blood flow and crush the tiny channels that carry bile and nutrients. The result? The liver slowly loses function.
Doctors divide cirrhosis into two stages: compensated and decompensated. In compensated cirrhosis, your liver is scarred but still managing to do its job. You might feel fine. No jaundice, no swelling, no confusion. But that doesn’t mean it’s safe. In decompensated cirrhosis, the liver can’t keep up anymore. Symptoms appear. Complications kick in. And that’s when the real danger starts.
What Causes It?
Not all liver damage leads to cirrhosis-but chronic damage almost always does. The big three causes today are:
- Alcohol-related liver disease: Drinking too much over years is still one of the top reasons. Even if you don’t consider yourself a heavy drinker, daily consumption adds up.
- Non-alcoholic fatty liver disease (NAFLD): This is now the fastest-growing cause in the U.S. and Australia. It’s linked to obesity, diabetes, and high cholesterol. What starts as fat buildup turns into inflammation, then fibrosis, then cirrhosis.
- Hepatitis B and C: Especially hepatitis C, which used to be the leading cause before effective antivirals came along. Many people had it for decades without knowing.
Other causes include autoimmune hepatitis, genetic conditions like hemochromatosis (too much iron), and bile duct diseases like primary biliary cholangitis. Some cases have no clear cause-called cryptogenic cirrhosis.
The key? It’s not about one bad night out. It’s about long-term, repeated injury. Your liver can handle occasional stress. But if the damage keeps coming-every day, every week, every year-it starts to break down.
How Do You Know You Have It?
Here’s the scary part: most people don’t feel anything until it’s advanced. Fatigue? Sure. But everyone gets tired. Upset stomach? Maybe indigestion. That’s why cirrhosis is often found by accident-during a routine blood test or ultrasound for something else.
When symptoms do show up, they’re serious:
- Ascites: Fluid builds up in the belly, making it swell. This is one of the most common and distressing signs.
- Jaundice: Skin and eyes turn yellow because the liver can’t process bilirubin.
- Hepatic encephalopathy: Toxins that should be filtered out build up in the brain. You get confused, forgetful, shaky hands (asterixis), or even fall into a coma.
- Bleeding easily: The liver stops making clotting factors. Bruises appear for no reason. Nosebleeds happen often.
- Swollen legs and ankles: Fluid leaks out of blood vessels because of high pressure in the portal vein.
Doctors use a mix of tools to diagnose it:
- Blood tests: High bilirubin, low albumin, high INR (clotting time), low platelets.
- Imaging: Ultrasound, MRI, or elastography can measure liver stiffness. A reading above 12.5 kPa strongly suggests cirrhosis.
- Biopsy: Still the gold standard, but less common now because non-invasive tests are accurate enough for most cases.
Doctors also use scoring systems like MELD (Model for End-Stage Liver Disease) and Child-Pugh to predict survival and decide who needs a transplant. MELD scores range from 6 to 40. A score above 15 means your risk of dying within a year without a transplant is high.
Can It Be Reversed?
This is where people get hopeful-and sometimes misled. Early fibrosis? Yes, sometimes it can be reversed. Stop drinking. Lose weight. Treat hepatitis C. Your liver can heal itself-if the damage isn’t too far gone.
But once cirrhosis is established? No medication can undo the scar tissue. That’s a hard truth. The goal shifts from reversal to stopping further damage and managing complications.
That’s why early detection matters so much. If you’re diagnosed with compensated cirrhosis, you still have time. Quit alcohol. Control diabetes. Get vaccinated for hepatitis A and B. Avoid NSAIDs like ibuprofen-they stress the liver. Eat less salt. Take prescribed diuretics. Follow up with a hepatologist every 6 months.
There’s no magic pill. But lifestyle changes can keep you out of the hospital for years.
When Transplantation Becomes Necessary
When cirrhosis reaches decompensated stage, survival drops sharply. About half of people with decompensated cirrhosis won’t make it past five years without a transplant.
Liver transplantation isn’t a cure-all, but it’s the only treatment that replaces the damaged organ. In the U.S., cirrhosis is the leading reason for liver transplants-about 40% of all cases.
Getting on the transplant list isn’t easy. You need to be sick enough to qualify, but healthy enough to survive surgery. That means:
- MELD score above 15 (often higher depending on the center)
- No active alcohol or drug use for at least 6 months
- No untreated cancer or severe heart/lung disease
- Ability to follow complex medical plans
The waiting list is long. In 2022, there were 14,300 people on the list in the U.S., but only 8,780 transplants were done. About 12% of people on the list die each year waiting.
Thankfully, new tech is helping. Normothermic machine perfusion keeps donor livers alive outside the body longer, making more organs usable. Some centers are even testing stem cell therapies and bioartificial livers as bridges to transplant-but these are still experimental.
After transplant, survival rates are good: over 80% at five years. But you’ll need to take anti-rejection drugs for life. Infections, kidney problems, and even new cancers are risks. Still, for many, it’s a second chance.

What Life Looks Like After Diagnosis
Living with cirrhosis isn’t about a quick fix. It’s about daily management.
Patients often need:
- Diet changes: Less than 2,000 mg of sodium per day. Protein may need to be limited if encephalopathy develops.
- Medications: Diuretics for fluid, lactulose or rifaximin for brain fog, beta-blockers to lower portal pressure.
- Regular monitoring: Blood tests every 3-6 months. Ultrasounds every 6 months to screen for liver cancer.
- Support systems: Many struggle with depression or anxiety. Counseling and patient groups (like the American Liver Foundation) help.
One patient in Melbourne shared on a liver disease forum: “I was diagnosed with compensated cirrhosis from hepatitis C. I didn’t feel sick. But after starting treatment and cutting out alcohol, my MELD score dropped from 18 to 9 in 18 months. I’m still alive because I listened.”
Another said: “The mental fog after transplant took six months to clear. People thought I was lazy. I wasn’t. My brain was healing.”
Access to care varies. Only 35% of rural U.S. counties have a hepatologist. In Australia, access is better in cities, but regional patients still face long waits. Multidisciplinary clinics-where hepatologists, dietitians, social workers, and addiction specialists work together-cut hospital readmissions by 40%.
What’s Changing in Cirrhosis Care?
The field is moving fast. Five years ago, we relied mostly on ultrasound elastography. Now, MR elastography is 90% accurate-better than biopsy in some cases.
New drugs are coming. Obeticholic acid is already approved for certain types of cirrhosis. Trials for drugs like simtuzumab show promise in slowing fibrosis in fatty liver-related cirrhosis.
The future? Personalized treatment. Instead of just staging cirrhosis as compensated or decompensated, doctors will soon look at molecular markers-the exact type of scarring, inflammation, and cell damage in your liver. That’ll tell us which treatments will work best for you.
But the biggest challenge remains: organ shortage. Until we can grow livers in labs or fully replicate their function, transplantation will stay the only definitive cure.
What You Can Do Now
If you’ve been told you have early liver damage:
- Get tested for hepatitis B and C.
- Stop drinking alcohol completely.
- Get your blood sugar and cholesterol checked.
- Ask your doctor about a liver stiffness scan.
- See a hepatologist, even if you feel fine.
If you’re already diagnosed with cirrhosis:
- Follow your treatment plan like your life depends on it-because it does.
- Get vaccinated for flu, pneumonia, and hepatitis A.
- Never take over-the-counter painkillers without checking with your doctor.
- Join a support group. You’re not alone.
Cirrhosis is not a death sentence. But it’s a wake-up call. The difference between living five years and living twenty often comes down to one thing: what you do after the diagnosis.
Can cirrhosis be cured with medication?
No, there is no medication that can reverse established cirrhosis. Scar tissue doesn’t go away. But stopping the cause-like alcohol or hepatitis-can prevent further damage and sometimes improve liver function enough to avoid transplant. Early-stage fibrosis may improve, but once cirrhosis is confirmed, the focus shifts to managing complications and preventing progression.
How long can you live with cirrhosis?
It depends on the stage. With compensated cirrhosis, many people live 10-15 years or more with proper care. Once decompensation happens-fluid buildup, bleeding, or brain fog-life expectancy drops to 2-5 years without a transplant. MELD score is the best predictor: higher scores mean higher risk.
Is liver transplant the only option for advanced cirrhosis?
For advanced cirrhosis with complications, yes-it’s the only treatment that replaces the damaged organ. Other treatments like diuretics, lactulose, or paracentesis manage symptoms but don’t fix the underlying problem. Transplantation offers the best chance for long-term survival. Experimental therapies like stem cells or bioartificial livers are in early trials but not yet standard.
Can you get cirrhosis without drinking alcohol?
Absolutely. In fact, non-alcoholic fatty liver disease (NAFLD) is now the fastest-growing cause of cirrhosis in countries like the U.S. and Australia. It’s linked to obesity, type 2 diabetes, and metabolic syndrome. Many people with NAFLD don’t even know they have it until cirrhosis is found on a routine scan.
What foods should you avoid with cirrhosis?
Avoid high-sodium foods: canned soups, processed meats, soy sauce, and fast food. Limit salt to under 2,000 mg per day. In advanced cases, too much protein can worsen brain fog, so your doctor may recommend moderate intake. Raw shellfish should be avoided due to infection risk. Alcohol is strictly prohibited.
How do you know if cirrhosis is getting worse?
Watch for new or worsening symptoms: swelling in the belly or legs, yellowing skin or eyes, confusion or forgetfulness, vomiting blood, or very dark stools. These signal decompensation. Regular blood tests and ultrasounds every 6 months help catch changes early. If you notice any of these, contact your doctor immediately.

Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.