When a patient picks up a prescription and sees a pill that looks completely different from what they’ve been taking, it’s natural to panic. The color is wrong. The shape is odd. The name on the bottle doesn’t match. For many, this isn’t just a change in appearance-it feels like a betrayal. And that’s where pharmacists step in. Not just to hand over the bottle, but to explain, reassure, and confirm understanding. Generic medication counseling isn’t optional. It’s a legal requirement, a clinical necessity, and often the difference between a patient staying on their treatment or stopping it altogether.
Why Generic Counseling Matters More Than You Think
Over 90% of prescriptions filled in the U.S. are for generic drugs. Yet, only a fraction of patients truly understand what that means. A 2023 Consumer Reports survey found that 43% of people believe generic medications are less effective. Nearly a third think they take longer to work. Almost 37% worry they cause more side effects. These aren’t just myths-they’re barriers to health.
One patient in the r/pharmacy Reddit thread shared how they stopped taking their blood pressure medication for two weeks because the generic looked different. They thought the pharmacy made a mistake. Another patient said their pharmacist showed them side-by-side photos of the brand and generic versions. That one-minute conversation saved them from throwing away their pills-and potentially risking a stroke.
These aren’t rare stories. Studies show that patients who receive clear, targeted counseling about generics are 68% more likely to trust their medication. Without it, non-adherence spikes. And non-adherence doesn’t just hurt the patient-it increases hospitalizations, emergency visits, and overall healthcare costs.
What the Law Actually Requires
Since 1990, federal law under OBRA ’90 has required pharmacists to counsel patients on all new prescriptions. That includes generics. But it’s not just federal. All 50 states have their own rules, and they vary.
In 32 states, pharmacists must specifically tell patients when a generic substitution is made. In 17, they only need to counsel if the patient asks. In others, the law is silent-leaving pharmacists to decide how much to say. This patchwork creates confusion, but one thing stays constant: the pharmacist is legally responsible for ensuring the patient understands what they’re taking.
The Centers for Medicare & Medicaid Services (CMS) makes it clear: “A patient’s complete understanding of how to use a prescription medication is critical to successful adherence.” That means you can’t just say, “Do you have any questions?” and call it done. You have to cover the basics-and the specifics.
The 5 Essential Points to Cover Every Time
There’s no one-size-fits-all script, but research and guidelines from the American Society of Health-System Pharmacists (ASHP) and the BC Pharmacists Association point to five non-negotiable points for every generic counseling session:
- Confirm the patient’s identity. Don’t assume you’re talking to the right person. Even small mistakes here can lead to dangerous mix-ups.
- Explain what generic substitution means. Say it plainly: “This is the same active ingredient as your brand, just made by a different company. It works the same way.”
- Describe the physical differences. “The brand was blue and oval. This one is white and round. That’s because the inactive ingredients-like fillers and dyes-are different. But the medicine inside? Identical.”
- Reaffirm bioequivalence and safety. Use simple language: “The FDA requires generics to be just as safe and effective as the brand. They go through the same strict testing.”
- Use the teach-back method. Ask the patient: “Can you tell me in your own words why you’re taking this and how you’ll take it?” If they can’t, you haven’t finished counseling.
This isn’t about reading from a checklist. It’s about making sure the patient walks away with zero doubt. A 2024 NIH study found that when pharmacists used teach-back, patient confidence in generics jumped from 32% to 68%.
Common Misconceptions (and How to Debunk Them)
Patients don’t come in with blank slates. They’ve heard things-from friends, TV, or online forums. Here’s what they’re thinking, and how to respond:
- “Generics aren’t as strong.” “They’re required by law to deliver the same amount of active ingredient within the same time frame as the brand. The FDA checks this for every batch.”
- “I had side effects last time-I think it’s the generic.” “Sometimes, side effects happen because the inactive ingredients (like dyes or preservatives) are different. That’s why we check your history. If you had a reaction before, we can look for a version without that ingredient.”
- “The brand worked better for me.” “Sometimes it’s psychological. But if you feel a real difference, we can document it and ask your doctor about staying on the brand-or trying another generic.”
Don’t dismiss concerns. Validate them. Then correct them with facts.
Time Is Short. How to Counsel Effectively Anyway
Pharmacists in community settings average just 1.2 minutes per counseling session. That’s not enough to explain bioequivalence, check for allergies, and teach back. So how do you do it?
Start with structure. Use a simple script you’ve practiced. Keep it conversational, not robotic. “You might notice this looks different from your last bottle. That’s because it’s the generic version. It’s the same medicine, just cheaper. Do you have any concerns about taking it?”
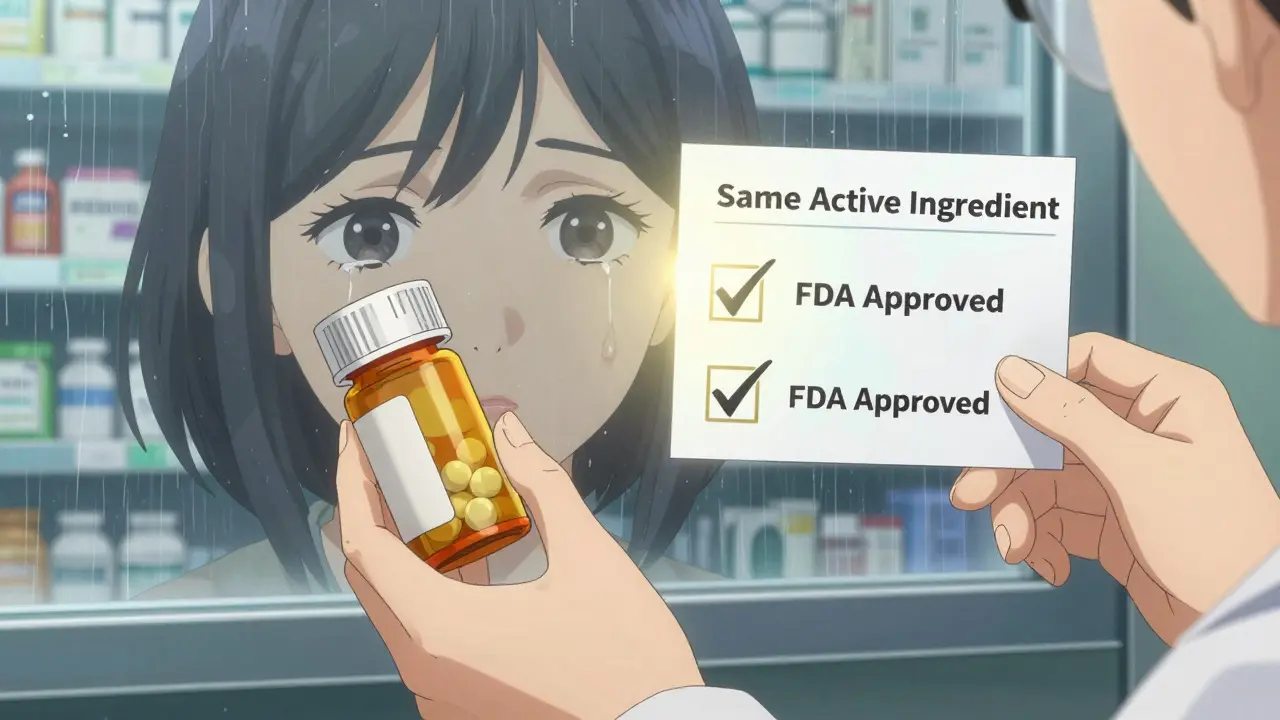
Use visual aids. Many pharmacies now have tablets or printed cards showing side-by-side images of brand and generic pills. A picture is worth a thousand words when someone’s anxious.
Let technology help. Over 68% of major pharmacy chains now use electronic prompts that pop up when a generic is dispensed. These remind pharmacists to cover key points without adding extra steps.
And never rely on technicians to do the counseling. Only pharmacists can legally provide it. Technicians can say, “The pharmacist will talk to you about your medication,” but they can’t explain bioequivalence.

Documentation Isn’t Red Tape-It’s Protection
Documentation requirements vary by state. In California, you must check a box confirming you discussed generic substitution. In Texas, you just note “counseling offered.” But starting in 2024, CMS is tightening the rules. Now, you must document what you discussed-not just that you did.
That means writing down things like: “Explained generic substitution. Patient concerned about pill appearance. Showed comparison image. Patient confirmed understanding.”
This isn’t busywork. It’s legal protection. It’s proof you did your job. And in a world where lawsuits over medication errors are rising, that matters.
The Bigger Picture: Why This Is About More Than Pills
Generic drugs save the U.S. healthcare system over $300 billion a year. But that savings means nothing if patients don’t take them. Counseling isn’t just about compliance-it’s about equity. Low-income patients, seniors on fixed incomes, and those on Medicare rely on generics to afford their care. If they stop because they’re scared, the cost isn’t just financial. It’s health. It’s life.
Every time you take those extra 90 seconds to explain a generic, you’re not just doing your job. You’re preventing hospitalizations. You’re reducing emergency visits. You’re giving someone peace of mind.
And that’s why, no matter how busy the day gets, you never skip it. You never rush it. You never assume they know.
What’s Changing in 2025 and Beyond
The future of generic counseling is evolving. By 2026, 75% of pharmacies are expected to use AI tools that flag patients with past concerns about generics-like those who switched brands multiple times or had refill gaps after a substitution. These tools will help pharmacists personalize their approach.
Medicare’s new quality metrics now include evidence of proper generic counseling as a factor for bonus payments. That means pharmacies that do it well will get rewarded. Those that don’t? They’ll fall behind.
But the biggest challenge? Administrative burden. Since 2020, pharmacists have spent 19% more time on documentation. The American Medical Association warns this could reduce actual patient time. That’s why simple, clear documentation templates are now critical.
The solution? Train your team. Use templates. Use tech. But never let efficiency replace empathy. Because in the end, patients don’t remember how fast you were. They remember if you made them feel safe.
Do I have to counsel every time a generic is dispensed?
Yes. Federal law under OBRA ’90 requires counseling for all new prescriptions, including generics. Most states also require counseling for refills. Even if the patient has taken the same generic before, you must confirm understanding each time. This isn’t just policy-it’s a legal requirement.
Can I just say, “This is the generic version” and be done?
No. Simply naming the drug as generic isn’t enough. Patients need to understand why it’s safe, why it looks different, and that it works the same. Without explaining bioequivalence and addressing appearance changes, you’re leaving room for misunderstanding-and potential non-adherence.
What if the patient refuses counseling?
You still have to offer it. If they refuse, document it clearly: “Counseling offered and declined by patient.” Some states require you to note their reason. Never assume refusal means understanding. Many patients say no because they’re in a hurry, not because they know what they’re taking.
Are generics really as safe as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also meet the same strict standards for purity and performance. The only differences are in inactive ingredients-which can affect appearance or taste, but not effectiveness.
How do I handle patients who speak little English?
Federal law requires language assistance under Title VI of the Civil Rights Act. Use professional interpreters-never family members. Many pharmacies have access to phone or video interpretation services. Have translated handouts ready for common generics. Never rely on Google Translate. Miscommunication here can be dangerous.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.