When your lungs start to feel heavy, your cough won’t quit, and breathing feels like a chore, it’s not just a cold. It could be pneumonia - a lung infection that sends over 1 million people to the hospital in the U.S. every year. But not all pneumonia is the same. The type you have - bacterial, viral, or fungal - changes everything: how you feel, how it’s diagnosed, and most importantly, how it’s treated.
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia hits fast. One day you’re fine, the next you’re running a high fever - maybe 104°F or higher - with chills, sharp chest pain, and a cough that brings up thick, yellow or green mucus. Sometimes, you’ll even see streaks of blood. Your lips or fingernails might turn blue because your body isn’t getting enough oxygen. The main culprit? Streptococcus pneumoniae is a bacterium responsible for over half of community-acquired pneumonia cases worldwide, especially in children and older adults. It’s so common that it’s behind 12.6% of severe pneumonia cases in kids under five. Other bacteria like Staphylococcus aureus, Haemophilus influenzae, and Mycoplasma pneumoniae (the cause of "walking pneumonia") also play big roles. On a chest X-ray, bacterial pneumonia looks like a solid white patch - often on just one side of the lung. That’s called lobar consolidation. Doctors hear it too: when they listen with a stethoscope, the affected area might be completely silent because the air sacs are filled with pus and fluid. Treatment? Antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin usually do the trick. For more serious cases or resistant strains, fluoroquinolones are used. The key? Start early. Delayed treatment raises the risk of complications - and death. About 5-7% of people hospitalized with bacterial pneumonia don’t survive.Viral Pneumonia: The Slow Burn
Viral pneumonia doesn’t come with a siren. It creeps in. You start with a runny nose, sore throat, maybe a low-grade fever. Then, over three to five days, it moves deeper. Your cough gets worse - dry at first, sometimes turning wet. You feel tired, achy, weak. Fever usually stays below 102°F. Influenza A and B are responsible for 20-30% of viral pneumonia cases, especially during flu season. RSV (respiratory syncytial virus) is a major cause in babies and older adults. SARS-CoV-2 (the virus behind COVID-19) also causes pneumonia - sometimes severe, sometimes mild. Other viruses like parainfluenza, rhinovirus, and human metapneumovirus add to the list. On an X-ray, viral pneumonia looks different. Instead of one solid white patch, you see a hazy, scattered pattern across both lungs. That’s called interstitial infiltrates - inflammation between the air sacs, not inside them. Antibiotics won’t help here. That’s critical. Taking them for a viral infection doesn’t cure anything - it just fuels antibiotic resistance. The CDC says 30% of outpatient antibiotic prescriptions are unnecessary, mostly because pneumonia gets misdiagnosed as bacterial when it’s viral. Treatment is mostly rest, fluids, and fever reducers. For flu, antivirals like oseltamivir (Tamiflu) can shorten the illness if taken within 48 hours. For severe COVID-19 pneumonia, remdesivir may be used. But the biggest danger? Secondary bacterial infections. About 25-30% of people with viral pneumonia - especially after the flu - develop a second, deadlier bacterial infection. That’s when things get serious fast.Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare - under 5% of cases - but it’s deadly for the wrong people. If you’re healthy, you probably won’t get it. But if you have HIV, are on chemotherapy, had an organ transplant, or take long-term steroids, your body can’t fight off these fungi. Coccidioides is the fungus behind Valley fever, common in the Southwest U.S., with 20,000 cases reported yearly. Histoplasma capsulatum hides in bird and bat droppings - soil where farmers, landscapers, or construction workers dig. Blastomyces dermatitidis lives in damp soil near rivers. You don’t catch it from people. You breathe in spores from the environment. Symptoms? Fever, cough with phlegm, night sweats, weight loss, even nausea. It can look exactly like bacterial or viral pneumonia - which is why it’s often missed. Chest X-rays might show nodules or patches, but they’re not always clear-cut. The only way to know? Special tests - sputum cultures, blood tests, or lung biopsies. And the treatment? Not antibiotics. Antifungals like amphotericin B or fluconazole. These drugs are stronger, slower, and come with more side effects than antibiotics. Mortality rates for fungal pneumonia in high-risk patients? 10-15%.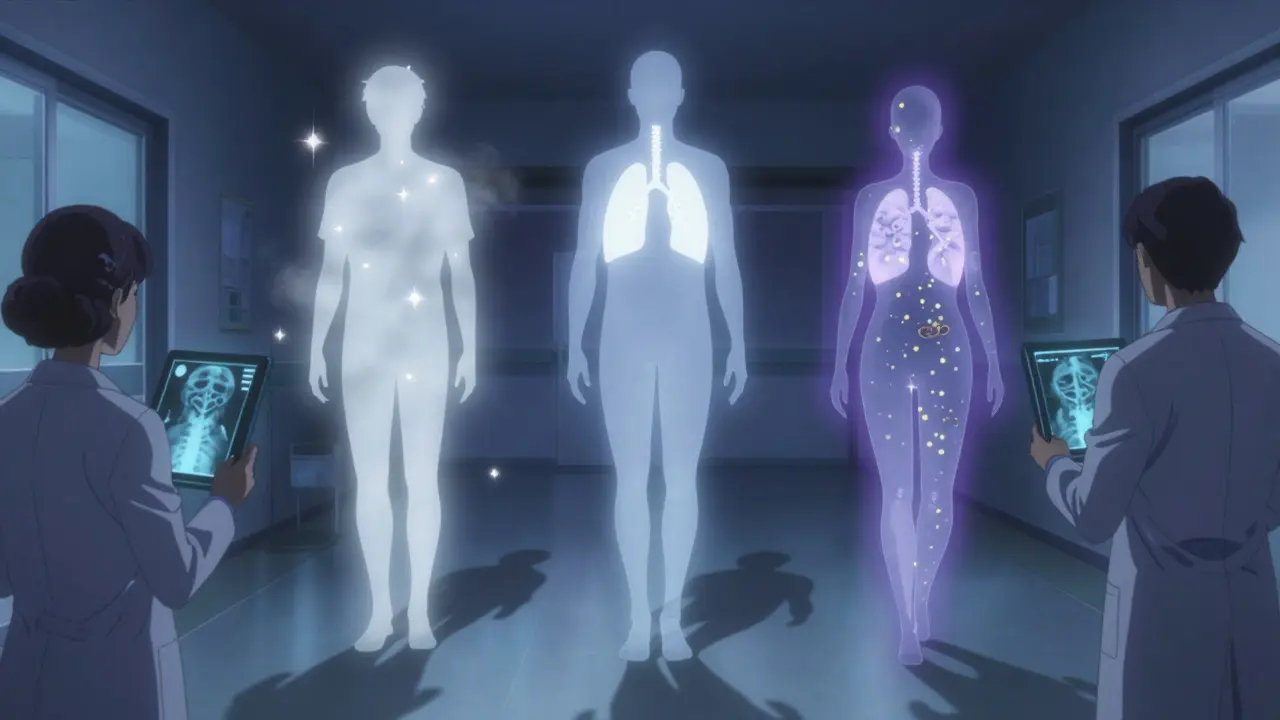
How to Tell Them Apart
It’s not always easy. But here’s what doctors look for:| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden (hours to 1 day) | Gradual (3-5 days) | Gradual (weeks) |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Moderate to high |
| Cough | Productive, colored mucus | Dry, worsening over time | Productive, sometimes bloody |
| Chest X-ray | One lobe, solid white patch | Bilateral, hazy, scattered | Nodules, patches, sometimes cavities |
| Primary Treatment | Antibiotics | Supportive care, antivirals if applicable | Antifungals |
| High-Risk Groups | Children, elderly, smokers | Infants, elderly, pregnant | Immunocompromised, farm/soil workers |
Prevention: What Actually Works
You can’t always avoid pneumonia - but you can lower your risk. For bacterial pneumonia, the pneumococcal vaccine reduces infection risk by 60-70% in children and 45-75% in adults over 65. The newer Prevnar 20 (20-valent) vaccine covers more strains and is now recommended for all adults 65+ and high-risk adults 19-64. For viral pneumonia, the flu shot cuts pneumonia risk by 40-60% in good match years. COVID-19 vaccines reduce pneumonia risk by up to 90% in the months after vaccination. For fungal pneumonia? Avoid dust in high-risk areas. Wear a mask if you’re digging in soil, cleaning chicken coops, or exploring bat caves. If you’re immunocompromised and live in an endemic region, talk to your doctor about preventive steps.
What Happens If You Get It Wrong?
Taking antibiotics for viral pneumonia doesn’t help - and it hurts. It kills good bacteria in your gut. It makes you more likely to get resistant infections later. And it contributes to a global crisis: antimicrobial resistance. The CDC says 35% more resistance develops in communities where antibiotics are misused. Missing fungal pneumonia? That’s even riskier. If you’re immunocompromised and treated with antibiotics for what you think is bacterial pneumonia, the fungus keeps growing. By the time it’s diagnosed, it’s often too late.What’s Next?
New tools are coming. Blood tests that check your body’s immune response - not just the pathogen - can now tell if an infection is bacterial or viral with over 90% accuracy. Multiplex PCR tests can screen for 20+ viruses and bacteria from one nasal swab in under 24 hours. The goal? Stop guessing. Start treating right - the first time.Can you have pneumonia without a fever?
Yes, especially in older adults, young children, or people with weakened immune systems. A low-grade fever or no fever at all doesn’t rule out pneumonia. Other signs - like confusion, rapid breathing, or extreme fatigue - may be the only clues.
Is pneumonia contagious?
The germs that cause pneumonia can be contagious, but pneumonia itself isn’t directly spread like a cold. You can catch the virus or bacteria from someone coughing or sneezing - and then develop pneumonia if your lungs get overwhelmed. That’s why flu season brings more pneumonia cases.
How long does pneumonia last?
Bacterial pneumonia often improves within 3-5 days of starting antibiotics, but full recovery can take weeks. Viral pneumonia may linger for 1-3 weeks, with fatigue lasting longer. Fungal pneumonia can take months to clear, especially in people with weak immune systems.
Can pneumonia come back after treatment?
Yes. If treatment was incomplete, the infection wasn’t fully cleared, or you have an underlying condition like COPD or diabetes, pneumonia can return. Reinfection is also possible - especially if you’re exposed again to the same germ.
Should I get tested if I think I have pneumonia?
If you have trouble breathing, chest pain, high fever, or symptoms lasting more than a week, see a doctor. A chest X-ray and possibly a blood test or sputum culture can confirm pneumonia and help identify the type. Don’t wait - early treatment saves lives.


Hi, I'm Caden Lockhart, a pharmaceutical expert with years of experience in the industry. My passion lies in researching and developing new medications, as well as educating others about their proper use and potential side effects. I enjoy writing articles on various diseases, health supplements, and the latest treatment options available. In my free time, I love going on hikes, perusing scientific journals, and capturing the world through my lens. Through my work, I strive to make a positive impact on patients' lives and contribute to the advancement of medical science.