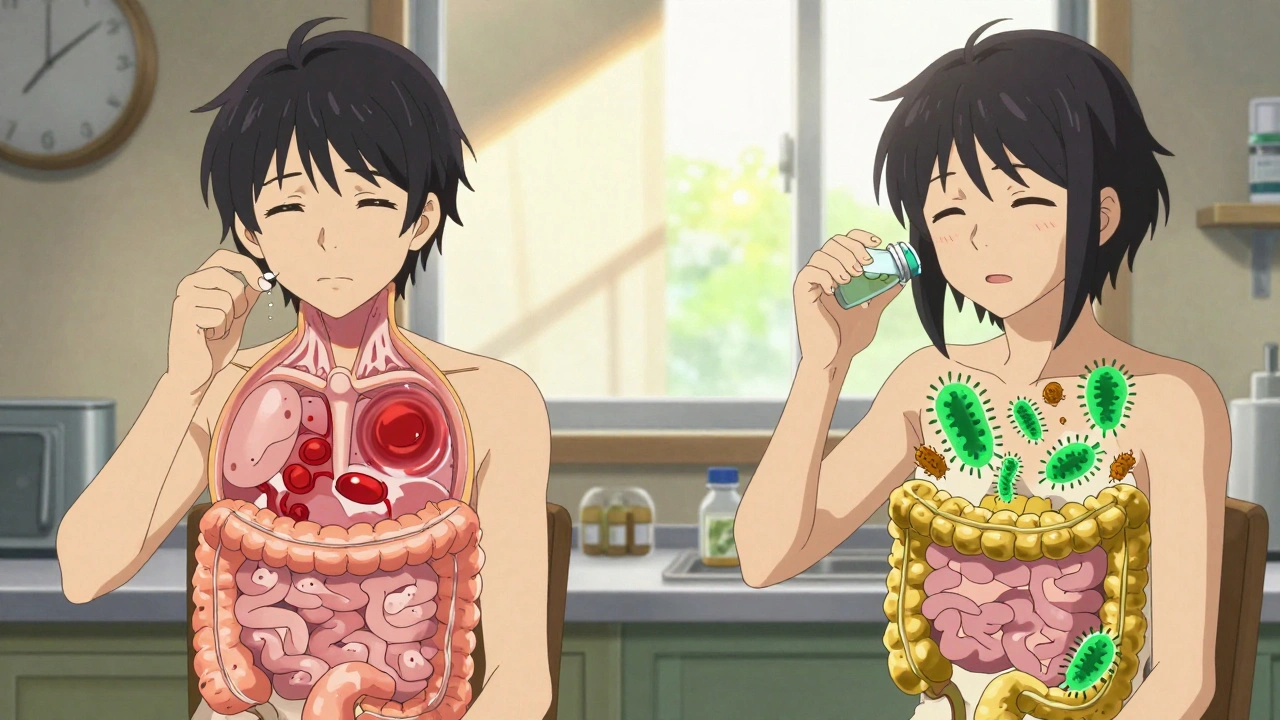
When you’re on antibiotics, your gut knows it. The good bacteria, the ones that help with digestion, immunity, and even mood, get wiped out along with the bad ones. That’s why so many people end up with diarrhea, bloating, or yeast infections after a course of antibiotics. The fix? Probiotics. But here’s the catch: if you take them at the wrong time, they won’t work.
Why Timing Matters More Than You Think
Antibiotics don’t pick and choose. They kill bacteria - including the helpful ones in your probiotic supplement. If you swallow a probiotic capsule right before or after your antibiotic pill, the antibiotic will likely kill those good bacteria before they even reach your gut. Studies show this can reduce probiotic survival by 78% to 92%. That’s not just a waste of money - it’s a missed chance to protect your gut.The solution isn’t complicated: space them out by at least two hours. This gives the antibiotic time to pass through your digestive system before the probiotic arrives. It’s not magic - it’s basic pharmacokinetics. Antibiotics peak in the gut within an hour or two and then start to clear. Two hours is the minimum buffer most clinical studies use to ensure probiotics survive.
Which Probiotics Work Best?
Not all probiotics are created equal. Some strains are tough enough to handle antibiotics. Others? Not so much.Saccharomyces boulardii is a yeast, not a bacteria. That means antibiotics don’t touch it. You can take this one at the same time as your antibiotic without losing effectiveness. It’s been shown to reduce antibiotic-associated diarrhea by 52% when taken at 20 billion CFUs per day.
For bacterial probiotics, stick to the well-researched strains:
- Lactobacillus rhamnosus GG (LGG) - proven to cut diarrhea risk by 47% at 10-20 billion CFUs per day
- Bifidobacterium lactis - helps restore balance after antibiotics
- Streptococcus thermophilus - often paired with LGG in clinical trials
Don’t fall for the “more strains = better” myth. A 2022 Cochrane Review found no significant difference between single-strain and multi-strain probiotics for preventing diarrhea. What matters is the strain, the dose, and the timing.
How Much Should You Take?
Dose matters. Too little, and you won’t see results. Too much, and you might just waste cash.Here’s what the science says:
- Mild cases (short antibiotic course, no past gut issues): 5-10 billion CFUs per day
- Moderate to severe (diarrhea, bloating, longer courses): 10-20 billion CFUs per day
- High-risk cases (14+ days of antibiotics, history of C. diff, IBD): 20-40 billion CFUs per day
Most over-the-counter probiotics only offer 1-5 billion CFUs. That’s not enough. Look for products that clearly list the strain and CFU count. Only 32% of commercial probiotics do this properly - so read the label like a detective.
When to Start - and When to Stop
Start as soon as possible. Don’t wait until you feel sick. The goal is prevention.Research from the NIH and the Journal of the American Medical Association shows that starting probiotics within 48 hours of your first antibiotic dose cuts the risk of diarrhea by 71% in kids and significantly lowers it in adults. Waiting until day 3 or later? You’re already behind.
And don’t stop when the antibiotics run out. Your gut needs time to rebuild. The International Scientific Association for Probiotics and Prebiotics (ISAPP) recommends continuing probiotics for 7 to 14 days after your last antibiotic pill. In one study, people who stuck with probiotics for 14 days post-antibiotics had 89% microbiome recovery - compared to just 63% in those who stopped early.

Real-Life Scheduling Examples
Let’s say your doctor prescribes amoxicillin - 500mg twice a day, at 8 a.m. and 8 p.m.Here’s how to space it:
- Take antibiotic at 8 a.m.
- Take probiotic at 10 a.m. or later - best at 10 a.m. or 6 p.m.
- Take antibiotic at 8 p.m.
- Take probiotic at 10 p.m. or 6 a.m. the next day
That’s two hours before or after - easy to remember. If you’re on a three-times-daily antibiotic, space probiotics 2 hours after each dose. Use phone alarms if you need to. Skipping doses cuts effectiveness by 37%, according to clinical data from Seed’s 2023 study.
What About Time-Release or Enteric Coated?
Newer probiotics use acid-resistant capsules or delayed-release tech to survive stomach acid and antibiotics. Companies like Seed and Pendulum are developing these. They’re promising - but not yet proven to eliminate the need for spacing.Even with these advanced formulas, most experts still recommend the 2-hour rule. Why? Because we don’t have enough long-term data yet. Until then, stick with what’s been tested in thousands of patients.
The Big Mistake Everyone Makes
Taking probiotics and antibiotics together. Right after each other. In the same pill. At breakfast.This is the #1 reason probiotics fail. It’s not that they don’t work - it’s that you’re killing them before they get a chance.
And it’s not just about diarrhea. Your gut microbiome loses 25-40% of its bacterial diversity during antibiotics. That’s not just a temporary upset - it can affect your immune system, your metabolism, even your mental health for months. Probiotics help. But only if they survive.

When to Be Cautious
Most people benefit from probiotics during antibiotics. But there are exceptions.Dr. Emeran Mayer from UCLA warns that in cases of severe broad-spectrum antibiotic use - like those used for hospital-acquired infections - probiotics might delay natural microbiome recovery in some people. This is still being studied. If you’re immunocompromised, have a central line, or are in the ICU, talk to your doctor first.
Also, if you’ve had a previous C. diff infection, probiotics are even more important - but only if you use the right strain (Saccharomyces boulardii is often recommended here).
What About Food and Probiotics?
You don’t need to take probiotics on an empty stomach. In fact, some studies suggest taking them with a small meal - especially one with healthy fats - can improve survival in the gut. Yogurt, kefir, or a spoon of olive oil with your probiotic won’t hurt. Just don’t mix it with your antibiotic.And forget about “gut healing” foods like bone broth or collagen. They sound nice, but they don’t replace the live bacteria you need. Stick to proven probiotic supplements with known strains and doses.
Final Checklist
Before you start your next antibiotic course, make sure you’ve got this covered:- Choose a probiotic with a proven strain (LGG or S. boulardii)
- Check the CFU count - aim for at least 10 billion per day
- Take it at least two hours apart from your antibiotic
- Start within 48 hours of your first antibiotic dose
- Keep taking it for 7-14 days after the antibiotics end
- Don’t skip doses - consistency matters more than the brand
If you do this right, you’re not just avoiding diarrhea. You’re protecting your long-term gut health - and that’s worth the extra effort.
Can I take probiotics at the same time as antibiotics?
Only if the probiotic is a yeast like Saccharomyces boulardii - it’s not affected by antibiotics. For bacterial probiotics like Lactobacillus or Bifidobacterium, taking them together kills up to 92% of the good bacteria. Always space them at least two hours apart.
How long should I take probiotics after antibiotics?
Continue for 7 to 14 days after your last antibiotic dose. Studies show this is when most gut microbiome recovery happens. Stopping too early means your good bacteria won’t fully bounce back.
Do I need a multi-strain probiotic?
No. Single-strain probiotics like Lactobacillus rhamnosus GG or Saccharomyces boulardii are just as effective - and often more reliable. Multi-strain products are marketed heavily, but clinical trials show no added benefit for preventing antibiotic-associated diarrhea.
What if I forget to space them?
If you accidentally take them together once, don’t panic. One mistake won’t ruin everything. Just go back to spacing them properly from the next dose. The key is consistency over time - not perfection.
Can I get probiotics from food instead of supplements?
Fermented foods like yogurt, kefir, sauerkraut, and kimchi contain probiotics, but they usually don’t have enough live bacteria or the right strains to match clinical doses. For reliable protection during antibiotics, supplements with labeled strains and CFUs are necessary.
Are probiotics safe for everyone?
For most healthy adults and children, yes. But if you’re immunocompromised, have a central IV line, or are critically ill, talk to your doctor first. In rare cases, probiotics can cause infections in vulnerable people.

I am a pharmaceutical expert with over 20 years of experience in the industry. I am passionate about bringing awareness and education on the importance of medications and supplements in managing diseases. In my spare time, I love to write and share insights about the latest advancements and trends in pharmaceuticals. My goal is to make complex medical information accessible to everyone.