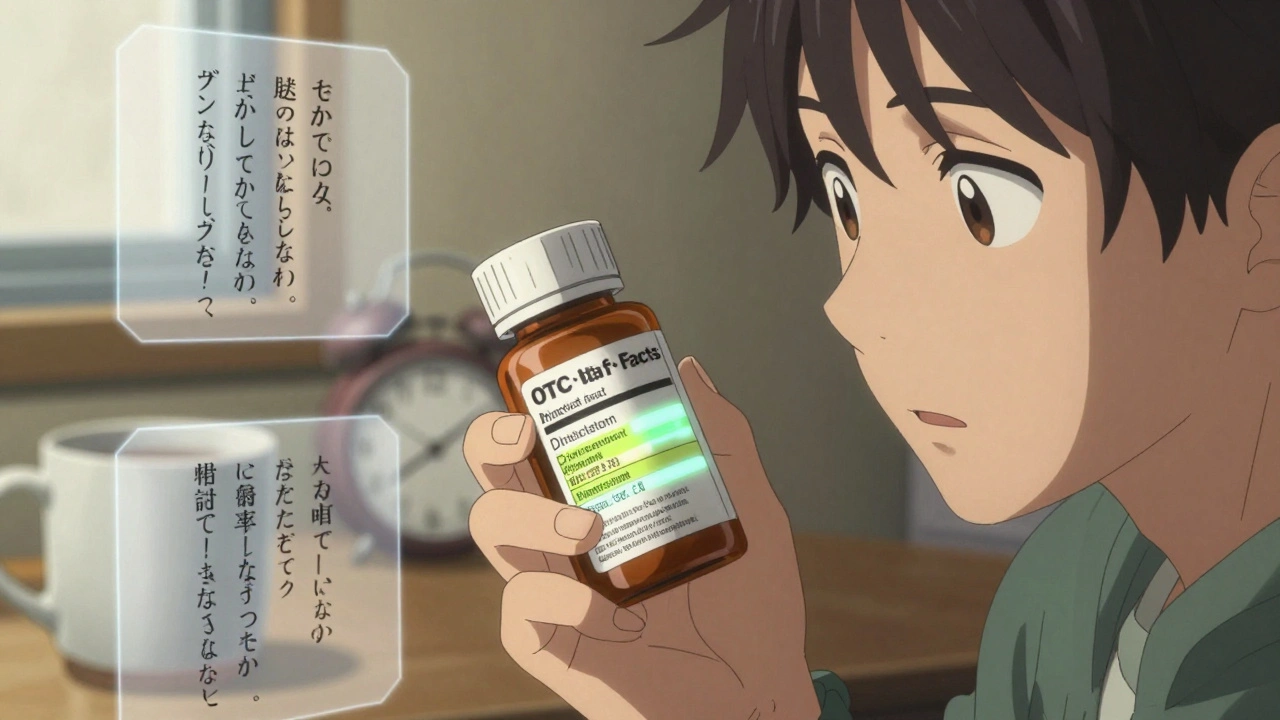
Learn how to read OTC Drug Facts labels to avoid dangerous mistakes, prevent overdoses, and use over-the-counter medicines safely. The FDA's standardized label helps you choose the right product and stay protected.
When you pick up a prescription, the drug labeling, the official printed information on a medication’s packaging and inserts that tells you how to use it safely. Also known as medication labeling, it’s the only legal document that tells you the right dose, the real risks, and what to avoid—yet most people never read it. The FDA requires every drug, whether brand-name or generic, to include specific details: active ingredients, dosage instructions, warnings, side effects, and storage rules. But here’s the problem: that tiny font on the side of the bottle? It’s often written for pharmacists, not patients. And if you’re taking multiple meds, missing one detail can lead to a dangerous interaction—or worse.
Drug labeling doesn’t just list facts—it shapes how you use medicine. For example, the FDA labeling guidelines, the strict rules that govern how drug makers present safety and usage info require black box warnings for the most dangerous drugs, like blood thinners or certain antidepressants. But you won’t see those warnings unless you open the insert. Meanwhile, generic drug labeling, the exact same info as the brand-name version, because the FDA requires bioequivalence is often printed smaller, with less space, making it harder to read. And if you’re using over-the-counter meds, the label might say "take with food"—but doesn’t explain why, or what happens if you skip it. That’s how people end up with stomach bleeds from NSAIDs or liver damage from too much acetaminophen.
Drug labeling also reveals hidden truths. Ever wonder why combo pills cost more than buying two separate generics? The label doesn’t say—but the FDA’s rules do. Generic manufacturers must match the brand’s bioequivalence, but they can still tweak inactive ingredients. That’s why some people react differently to generics—because the label doesn’t list fillers like lactose or dyes, which can trigger allergies or affect absorption. And when it comes to medication safety, the practice of using drugs correctly to avoid harm, the label is your first and last line of defense. A missed warning about caffeine interacting with warfarin? A confused dosage for infant drops? A label that says "take once daily" but doesn’t specify morning or night? These aren’t oversights—they’re risks built into the system.
Real people get hurt because they trust the bottle instead of reading it. One woman took clindamycin for a tooth infection and ignored the small print about C. diff—by the time she got to the ER, her colon was inflamed. Another man mixed melatonin with his blood pressure pill because the label didn’t mention interaction risks. These aren’t rare cases. They’re the result of labels that assume you already know how to read them. The truth? Drug labeling isn’t designed to be easy. It’s designed to be legally complete. That’s why you need to treat it like a manual—not a suggestion. The next time you get a new prescription, don’t just stash the insert. Read it. Highlight the warnings. Ask your pharmacist to explain the parts that don’t make sense. Because in the end, no AI, no app, no nurse can replace the power of knowing exactly what’s on that label—and what it means for your body.
Below, you’ll find real stories and facts about how drug labeling affects everything from antibiotic safety to generic drug effectiveness—and what you can do to make sure it works for you, not against you.
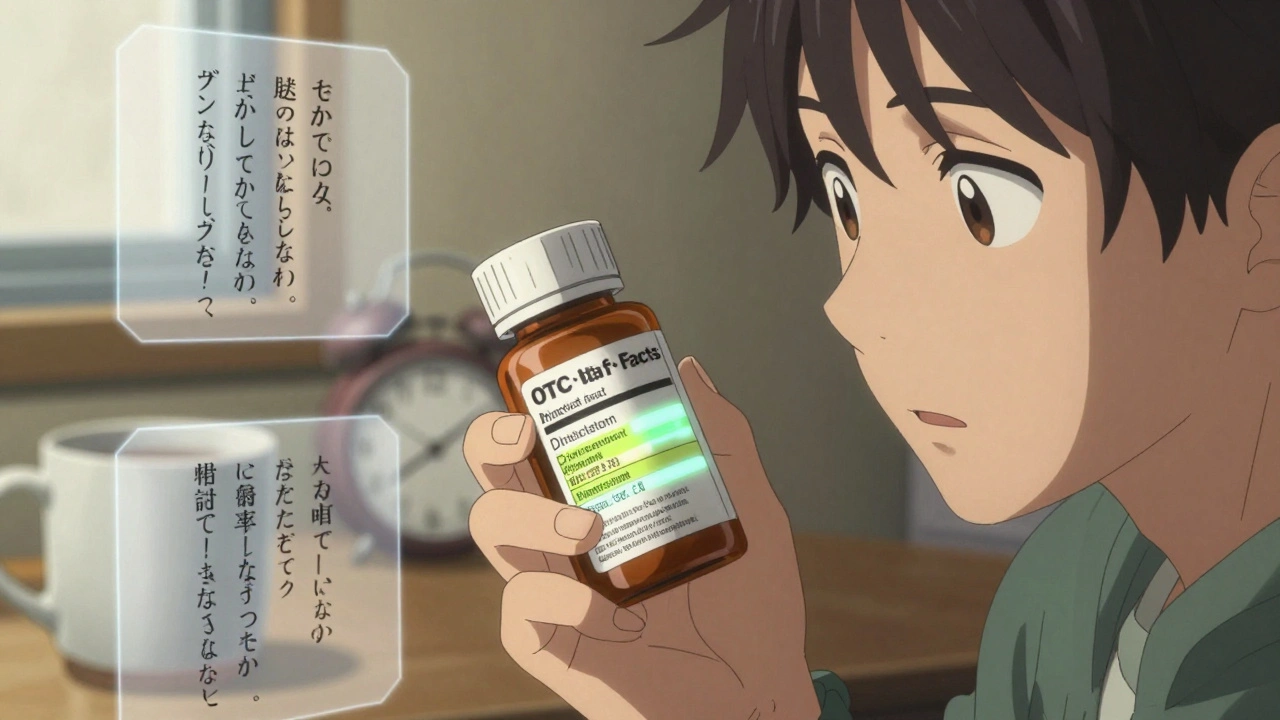
Learn how to read OTC Drug Facts labels to avoid dangerous mistakes, prevent overdoses, and use over-the-counter medicines safely. The FDA's standardized label helps you choose the right product and stay protected.