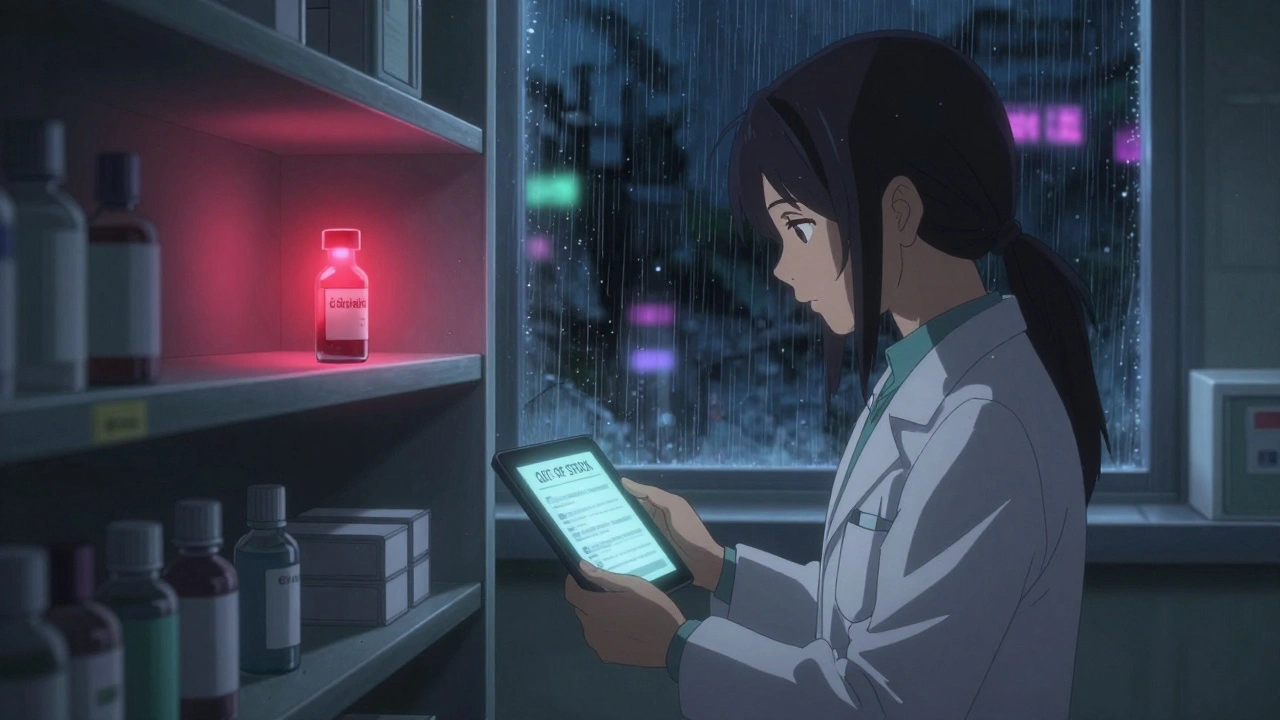
As of 2025, over 270 medications are in short supply in the U.S., including critical drugs like cisplatin, IV fluids, and GLP-1 weight-loss agents. Learn which drugs are hardest to find, why shortages keep happening, and what you can do.
When your pharmacy says generic drug shortages, a situation where affordable versions of common medications aren’t available in sufficient quantities. Also known as medication shortages, it’s not just an inconvenience—it’s a health risk. Millions rely on generics for blood pressure pills, antibiotics, thyroid meds, and even insulin. When these drugs vanish from shelves, people delay treatment, switch to costlier brands, or go without. And it’s not random—it’s systemic.
These shortages aren’t caused by lack of demand. They happen because the system is built on razor-thin profits. Most generic drugs sell for pennies. Companies make money by producing huge volumes, but that means they cut corners: one factory makes 80% of the active ingredient for a common antibiotic, and if that factory has a quality issue, the whole country runs out. pharmaceutical supply, the network of manufacturers, distributors, and regulators that get drugs from labs to patients is fragile. It depends on a few overseas plants—mostly in India and China—that face delays from inspections, raw material shortages, or even weather. When one link breaks, the whole chain stumbles.
drug supply chain, the path a medication takes from raw chemicals to your medicine cabinet isn’t designed for resilience. It’s built for efficiency. That means no backup suppliers, no extra stockpiles, and little transparency. When a shortage hits, pharmacies don’t know when the next shipment arrives. Doctors don’t always know what alternatives exist. And patients? They’re left guessing. Some shortages last weeks. Others drag on for months. Drugs like levothyroxine, metformin, and amoxicillin have all been hit hard in recent years—not because they’re rare, but because making them isn’t profitable enough to justify the risk.
It’s not just about running out of pills. Shortages force dangerous swaps. A patient switched from one generic blood pressure drug to another might get different absorption rates—something the 80-125% bioequivalence rule doesn’t always catch in real life. Or someone might be given a combo pill when they’d be better off with separate generics, costing them hundreds extra. These aren’t theoretical problems. They show up in ER visits, hospitalizations, and lost workdays.
You can’t fix the system alone, but you can protect yourself. Know which drugs you take are most likely to be affected. Ask your pharmacist if there’s a backup. Keep a list of your meds and dosages. If your drug disappears, don’t wait—call your doctor early. And if you’re on something like warfarin or lithium, where tiny changes matter, don’t switch without testing. The posts below show real cases: how combo generics cost more than buying separate pills, how bioequivalence rules work (and where they fall short), and how global supply chains make or break your access to basic meds. You’ll find practical tips on what to do when your prescription vanishes, how to spot unsafe substitutions, and how to advocate for yourself when the system fails.
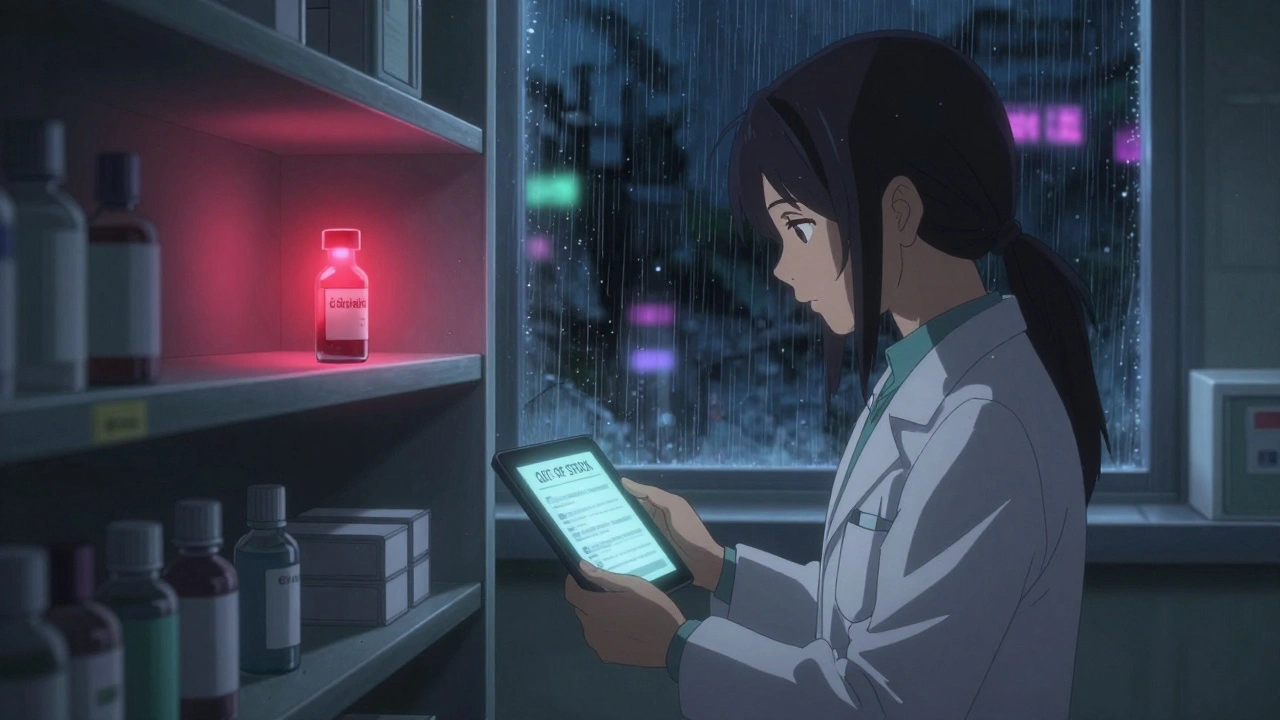
As of 2025, over 270 medications are in short supply in the U.S., including critical drugs like cisplatin, IV fluids, and GLP-1 weight-loss agents. Learn which drugs are hardest to find, why shortages keep happening, and what you can do.