Learn how INR monitoring keeps you safe on warfarin, what your target range should be, and how home testing compares to lab visits. Understand the risks of high and low INR levels and how to manage them.
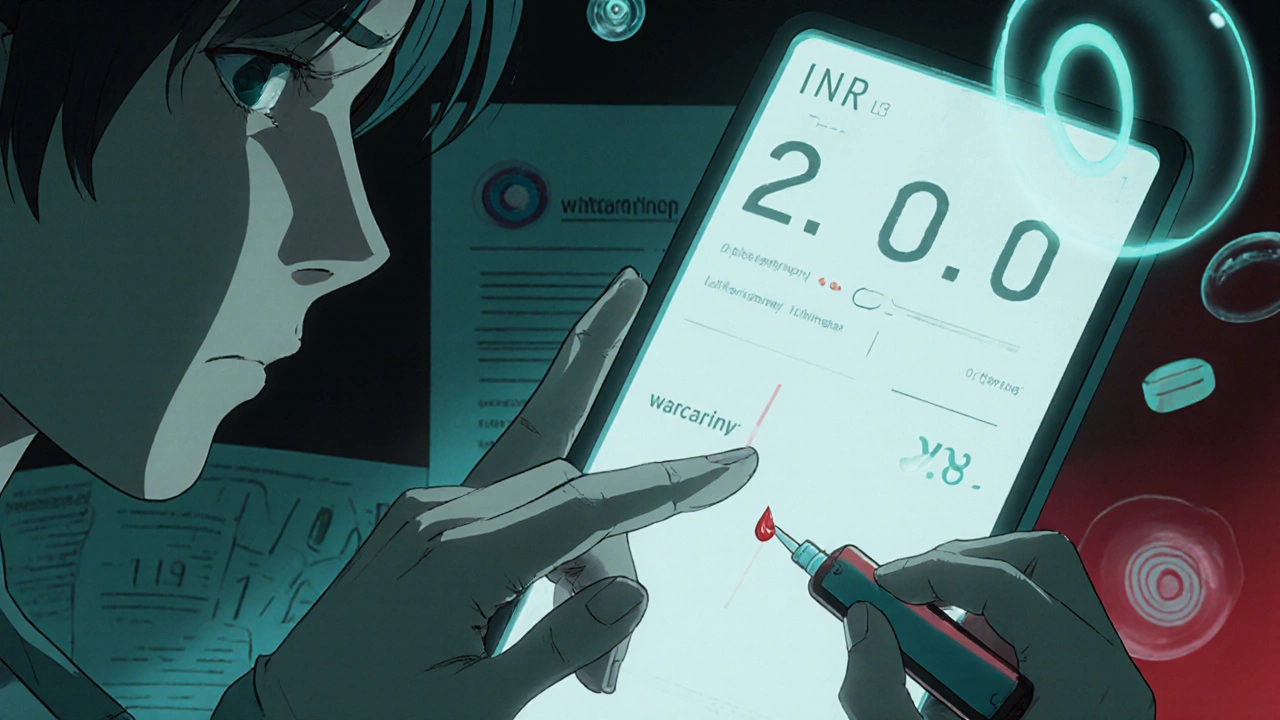
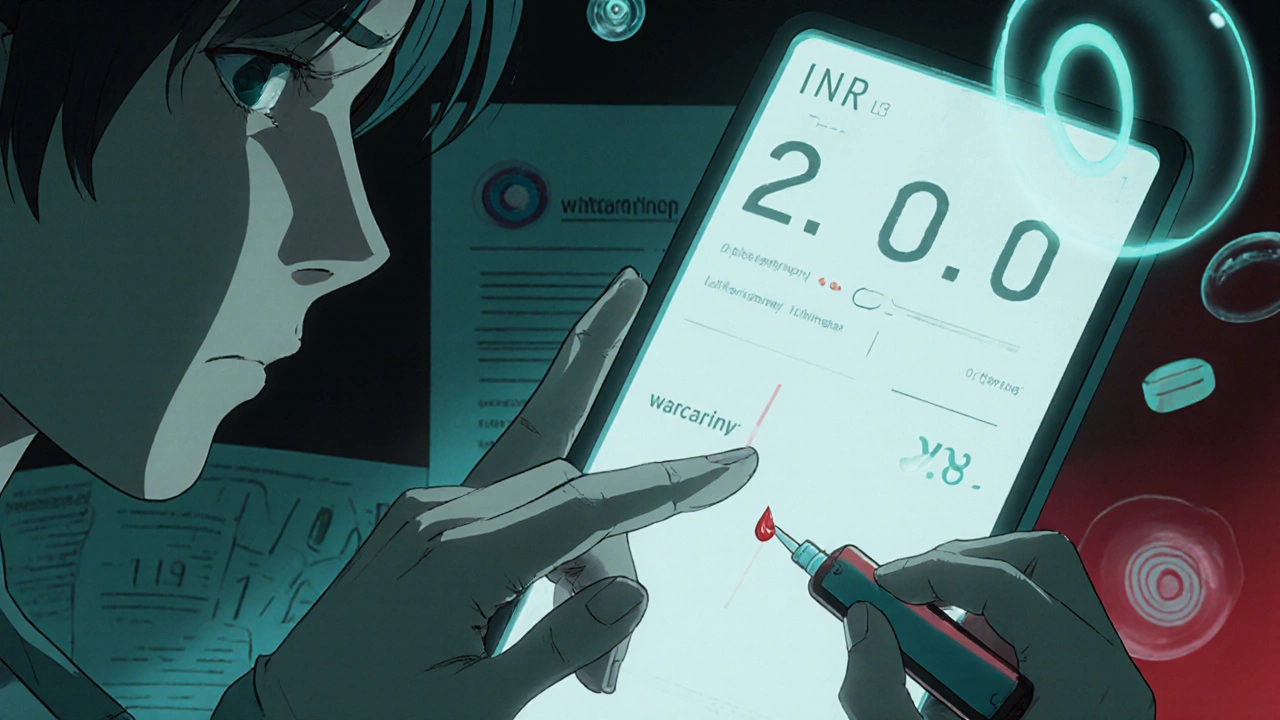
When you're on warfarin, a blood thinner used to prevent dangerous clots in people with atrial fibrillation, artificial heart valves, or a history of deep vein thrombosis. Also known as Coumadin, it works by slowing down your body’s ability to form clots—but it’s not a set-it-and-forget-it drug. Your warfarin levels aren’t measured by a simple blood concentration like some meds. Instead, doctors track something called the INR—International Normalized Ratio. This number tells you how long it takes your blood to clot. Too high, and you risk bleeding inside your brain or gut. Too low, and you could still get a stroke or a pulmonary embolism.
Keeping your INR in the right zone—usually between 2.0 and 3.0 for most people—isn’t just about taking your pill daily. It’s about what you eat, what else you take, and even how your liver is feeling that week. INR tests, a routine blood test used to monitor the effectiveness of anticoagulant therapy like warfarin are your lifeline. You might get them weekly at first, then every few weeks once things stabilize. But even small changes can throw things off. Eating a big bowl of spinach? That’s vitamin K, and it fights warfarin. Starting a new antibiotic? That can spike your INR. Taking Dong Quai or St. John’s Wort? Those herbal supplements can make warfarin either too strong or too weak. Even skipping a meal or drinking alcohol regularly can shift your levels.
And it’s not just you managing this. Your doctor, pharmacist, and even your dietitian need to be on the same page. That’s why so many of the articles in this collection focus on anticoagulant therapy, the medical use of drugs like warfarin and DOACs to prevent harmful blood clots and how they interact with other meds, foods, and conditions. You’ll find real-world stories about people who had to adjust their warfarin dose after switching antibiotics, or how someone’s INR crashed after starting a new supplement. You’ll see why some patients do better on DOACs instead, and why others stick with warfarin because it’s cheaper, or because they have a mechanical valve.
There’s no magic number that works for everyone. Your target INR might be different if you have a mechanical mitral valve versus atrial fibrillation. Your age, weight, kidney function, and even genetics play a role. That’s why understanding your own pattern matters more than memorizing a range. Keep a log. Note every dose, every new pill, every big change in your diet. Bring it to your appointments. The goal isn’t perfection—it’s awareness. Because when you know how your body responds to warfarin, you’re not just taking a pill. You’re actively protecting your life.
Below, you’ll find practical guides on how warfarin interacts with common medications, herbal supplements, and even everyday habits. Some posts dive into why certain foods mess with your levels. Others compare warfarin to newer options. There’s even advice on what to do if you miss a dose or your INR comes back too high. This isn’t theory. These are real experiences, real data, and real solutions from people who’ve been there.
Learn how INR monitoring keeps you safe on warfarin, what your target range should be, and how home testing compares to lab visits. Understand the risks of high and low INR levels and how to manage them.