Learn how to space probiotics and antibiotics correctly to prevent diarrhea and protect your gut health. Discover the right strains, doses, and timing backed by clinical research.
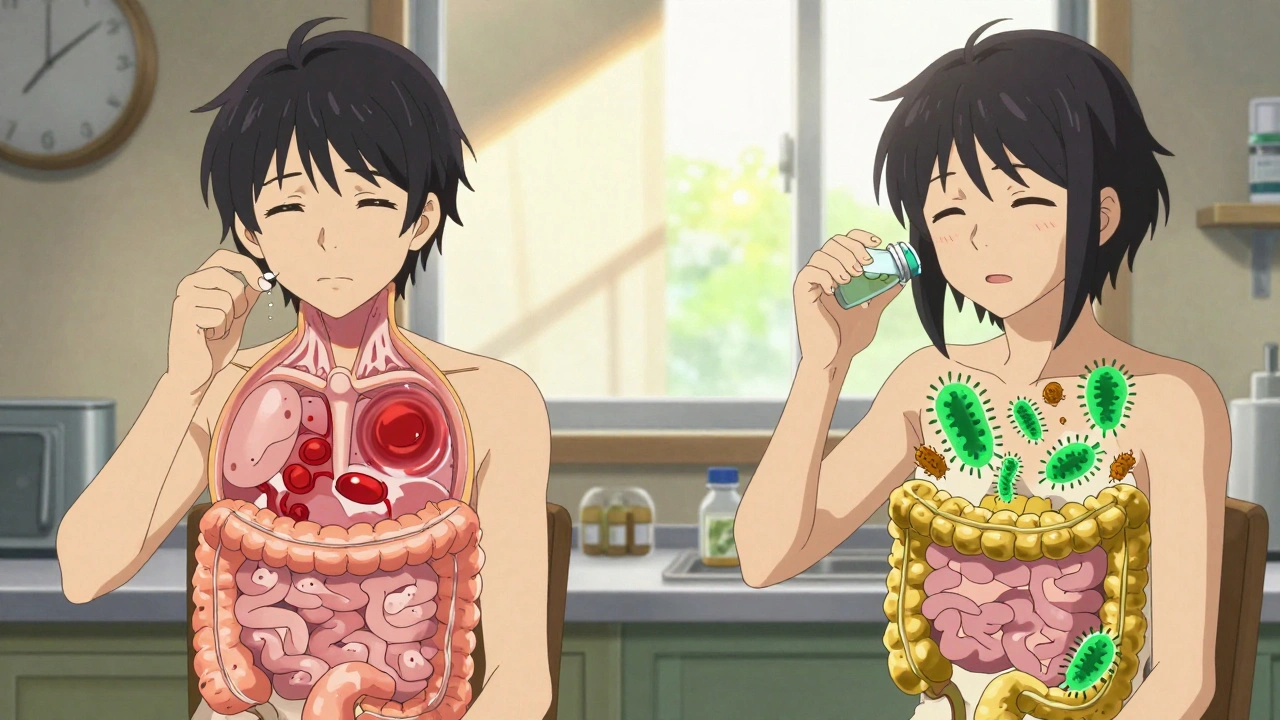
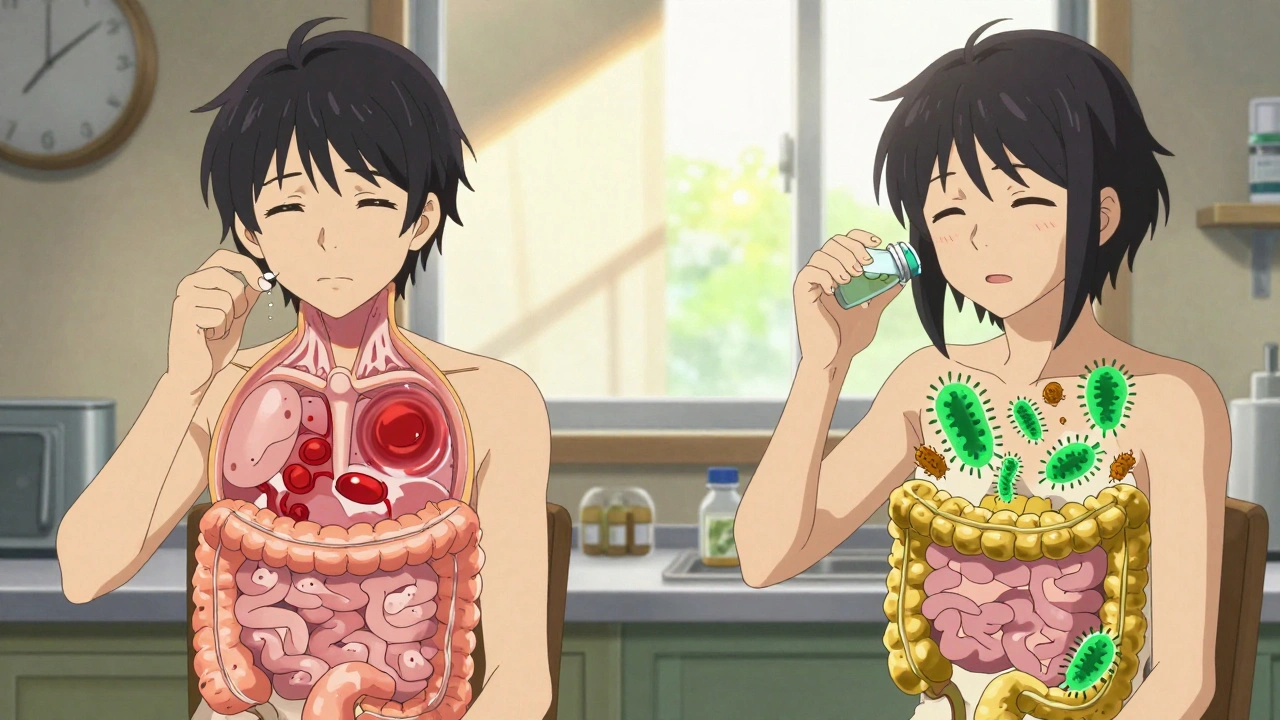
When you take an antibiotic-associated diarrhea, a common side effect caused by antibiotics disrupting the natural balance of bacteria in your gut. It’s not just an upset stomach—it’s your digestive system reacting to the loss of good bacteria that normally keep harmful ones in check. This isn’t rare. About 1 in 5 people who take antibiotics end up with loose stools, and for some, it’s far worse than just discomfort.
The biggest concern? C. difficile, a dangerous bacterium that can take over when antibiotics wipe out protective gut flora. This infection causes severe, watery diarrhea, fever, and even life-threatening colon damage. Clindamycin, a commonly prescribed antibiotic for skin and respiratory infections, carries one of the highest risks. But it’s not just clindamycin—amoxicillin, cephalosporins, and fluoroquinolones can trigger it too. The problem isn’t the antibiotic itself, but how it clears out the good bacteria that keep your gut stable.
Not everyone who gets diarrhea after antibiotics has C. difficile. Sometimes it’s just a mild, temporary imbalance. But if you’re having more than three watery stools a day, especially with cramping, fever, or blood in your stool, you need to act. Waiting it out can be dangerous. Your doctor can test for C. difficile with a simple stool sample, and early treatment stops it from turning into a hospital emergency.
What makes this even trickier is that the symptoms can show up weeks after you finish your antibiotics. You might think you’re in the clear—until your gut rebels. That’s why it’s not just about what you take, but how long the effects last. Some people get diarrhea on day two. Others don’t notice it until they’re done with the pills and back at work. That delay means many don’t connect the dots.
And it’s not just about stopping the antibiotic. Probiotics can help, but not all are equal. Some strains, like Saccharomyces boulardii and certain Lactobacillus species, have real evidence backing them for prevention. But they’re not magic pills—you still need to watch for warning signs. Hydration matters too. Losing fluids fast can land you in the ER, especially if you’re older or have other health issues.
Most people don’t realize how common this is, or how easily it’s mistaken for a stomach bug. You take an antibiotic for a sinus infection, feel fine for a few days, then start having diarrhea. You blame the takeout. But if you’ve been on antibiotics recently, it’s not the food—it’s the drug. That’s why awareness matters. Knowing the risks helps you ask the right questions before you even fill the prescription.
The posts below give you real, practical details you won’t find in a drug leaflet. You’ll see which antibiotics are most likely to cause trouble, what symptoms to never ignore, how to protect your gut during and after treatment, and what to do if things get serious. No fluff. No guesswork. Just what you need to stay safe when antibiotics enter your system.
Learn how to space probiotics and antibiotics correctly to prevent diarrhea and protect your gut health. Discover the right strains, doses, and timing backed by clinical research.