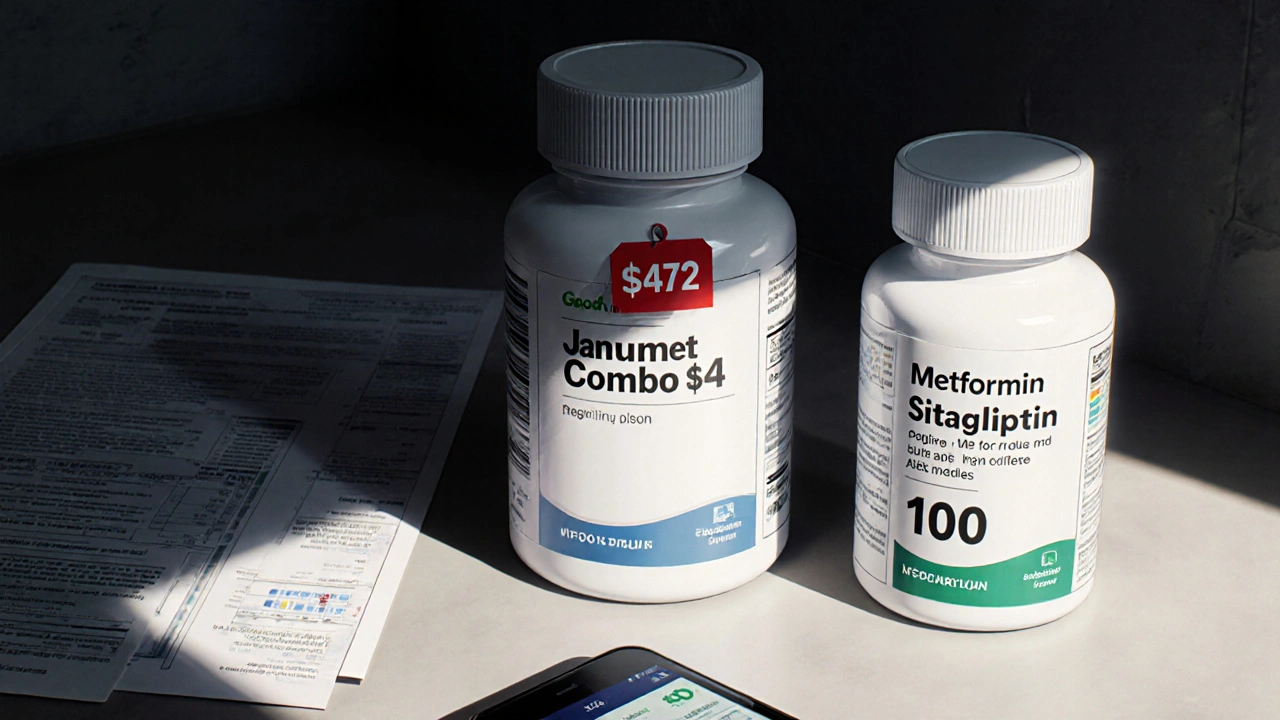
Combo generics often cost 3-4 times more than buying the same drugs as separate generics. Real data shows billions in wasted spending - here’s how to save hundreds per month.
When it comes to your health, medication safety, the practice of using drugs correctly to avoid harm while getting the intended benefit. Also known as drug safety, it’s not just about taking pills on time—it’s about knowing what they do, who they affect, and what they might be doing to you behind the scenes. In November 2025, we dug into the real-world risks most people never talk about: how a cup of coffee can wreck your warfarin levels, why using a kitchen spoon to dose your baby could land you in the ER, and how combo generics are secretly costing you hundreds every month.
Drug interactions, when two or more substances change how each other works in your body. Also known as medication conflicts, they’re not rare—they’re common, and often deadly. Caffeine doesn’t just keep you awake; it can make your thyroid meds useless or turn your blood thinner into a time bomb. Dong Quai, sold as a "natural" remedy, doubles your bleeding risk when mixed with warfarin. And it’s not just herbs—heatwaves, altitude, and even common illnesses can turn a safe dose into an overdose by changing how your body handles drugs. Meanwhile, INR monitoring, the regular blood test that tracks how thin your blood is on anticoagulants like warfarin. Also known as anticoagulation tracking, it’s the only thing standing between you and a stroke or internal bleed. Skip it once, and you’re gambling with your life.
Pediatric medication dosing, the precise measurement of liquid drugs for babies and young children. Also known as baby medicine safety, it’s one of the most overlooked dangers in home care. A single drop too much acetaminophen can cause liver failure. A teaspoon from your kitchen? That’s not a dose—it’s a lottery ticket. And it’s not just parents—nurses, grandparents, and even some pharmacies still get this wrong. Then there’s the money side: generic drugs, low-cost versions of brand-name medications that work the same way. Also known as off-patent drugs, they’re supposed to save you money—but when sold as combo pills, they often cost three times more than buying the same pills separately. You’re not saving. You’re being overcharged. And no one’s telling you.
These aren’t theoretical risks. They’re real, documented, and happening right now—to your neighbor, your sister, your aunt. We looked at how clindamycin triggers deadly gut infections, why montelukast helps some asthma patients but not others, and how inhaler mistakes cause hospital visits that could’ve been avoided. We broke down how NTI generics—drugs with zero room for error—are regulated differently across countries, and why that matters if you’re taking lithium or clozapine. We showed how lab calendars keep people alive on blood thinners, and how prescription assistance programs can help… or trap you in a cycle of dependency.
This isn’t a list of random articles. It’s a map of where things go wrong—and how to fix them. Whether you’re managing your own meds, caring for a child, or helping an aging parent, what you’ll find below isn’t theory. It’s what works. What saves money. What saves lives.
Combo generics often cost 3-4 times more than buying the same drugs as separate generics. Real data shows billions in wasted spending - here’s how to save hundreds per month.

Heatwaves increase overdose risk by dehydrating the body, intensifying drug effects, and reducing respiratory function. Learn practical harm reduction steps, how communities are responding, and what to do if someone overdoses during extreme heat.

Caffeine can interfere with common medications like warfarin, levothyroxine, and antidepressants, leading to dangerous side effects or reduced effectiveness. Learn which drugs interact with coffee, energy drinks, and other caffeine sources - and how to stay safe.

Montelukast is a daily oral medication that blocks leukotrienes to prevent asthma and allergy symptoms. It's not a rescue drug, but helps those who can't use inhalers or have both asthma and nasal allergies. Learn how it works, who benefits, and what to watch for.

Learn the 8 essential steps to use your inhaler correctly so medicine reaches your lungs, not your throat. Fixing your technique can cut side effects, prevent hospital visits, and make your treatment work as it should.

Never use household spoons to measure children's medicine. Kitchen spoons vary in size and can lead to dangerous overdoses or underdoses. Always use an oral syringe marked in milliliters for accurate, safe dosing.

Lab monitoring calendars help prevent dangerous side effects from medications like clozapine, lithium, and warfarin by tracking blood tests and symptoms on a schedule. Missing tests can lead to serious health risks-here’s how to stay on track.

Clindamycin increases the risk of C. difficile infection, a serious condition causing severe diarrhea and colon damage. Learn the warning signs, when to seek care, and how to avoid complications after taking this high-risk antibiotic.

Infant medication safety depends on accurate dosing, correct concentrations, and proper measuring tools. Learn how to avoid deadly errors with acetaminophen, ibuprofen, and other liquid meds for babies under 1 year.
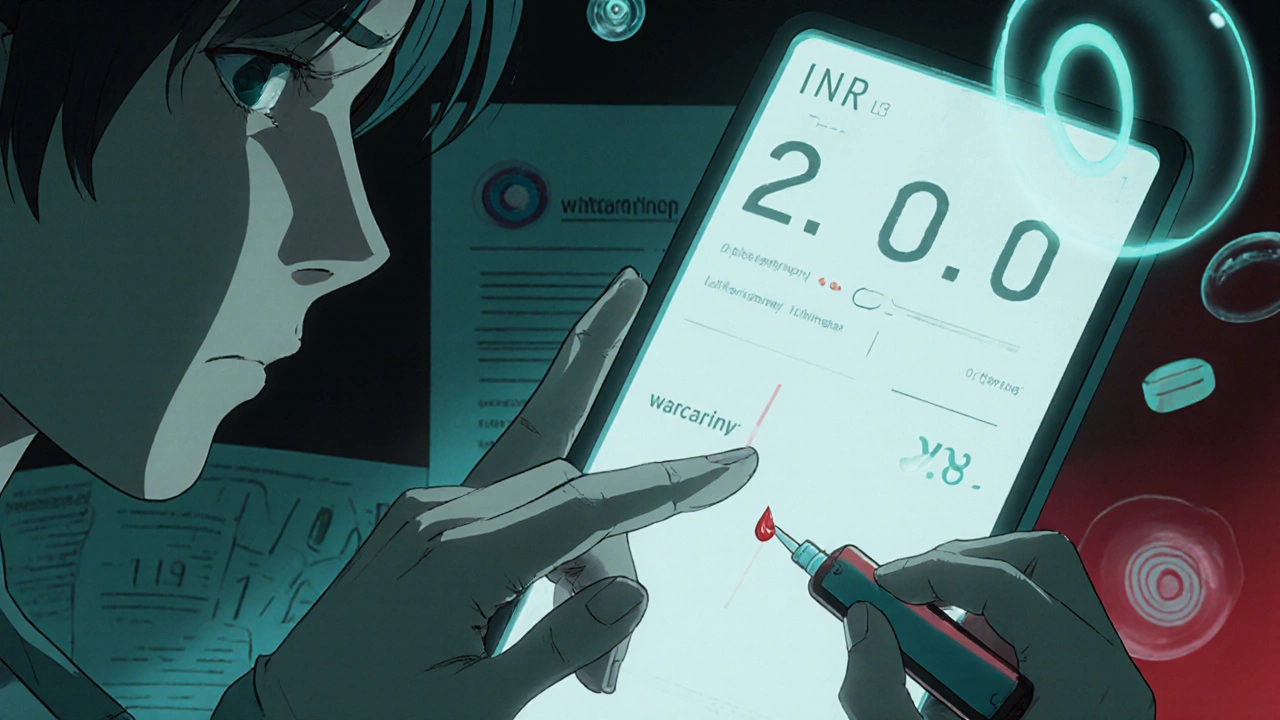
Learn how INR monitoring keeps you safe on warfarin, what your target range should be, and how home testing compares to lab visits. Understand the risks of high and low INR levels and how to manage them.